Electronic Health Record (EHR) software is transforming the way healthcare systems manage patient data. From improving diagnosis accuracy to ensuring compliance with standards like HIPAA, developing a robust, secure, and user-friendly EHR system is critical for modern healthcare providers. This article dives into the technical architecture, must-have features, regulatory compliance, design challenges, and strategic business value of custom EHR software development.
EHR (Electronic Health Record) Software Development
An Electronic Health Record (EHR) is essentially a digital version of a patient’s paper chart, encompassing the patient’s medical history, diagnoses, medications, immunizations, lab results, and more.
EHR software provides a secure, real-time, and patient-centered repository of this information, accessible instantly to authorized users across different healthcare settings.
In simpler terms, an EHR system enables doctors, nurses, pharmacists, and other providers to enter and retrieve up-to-date patient data through computers and mobile devices, replacing traditional paper records.
EHR software is fundamental to modern healthcare operations. Over the past decade, hospitals and clinics worldwide have rapidly adopted EHR systems due to their proven benefits.
In the United States, for example, EHR adoption among hospitals climbed from around 72% in 2012 to 96% of hospitals by 2021 after government incentives and industry pressure made digital records the norm.
Similar trends are seen globally as healthcare providers recognize that digital record-keeping improves efficiency, care coordination, and outcomes. Governments and health systems have heavily invested in EHR infrastructure – the global EHR market size, valued at about $27 billion in 2023, is projected to reach over $40 billion in the next decade.
Read: Healthcare Appointment Scheduling Software
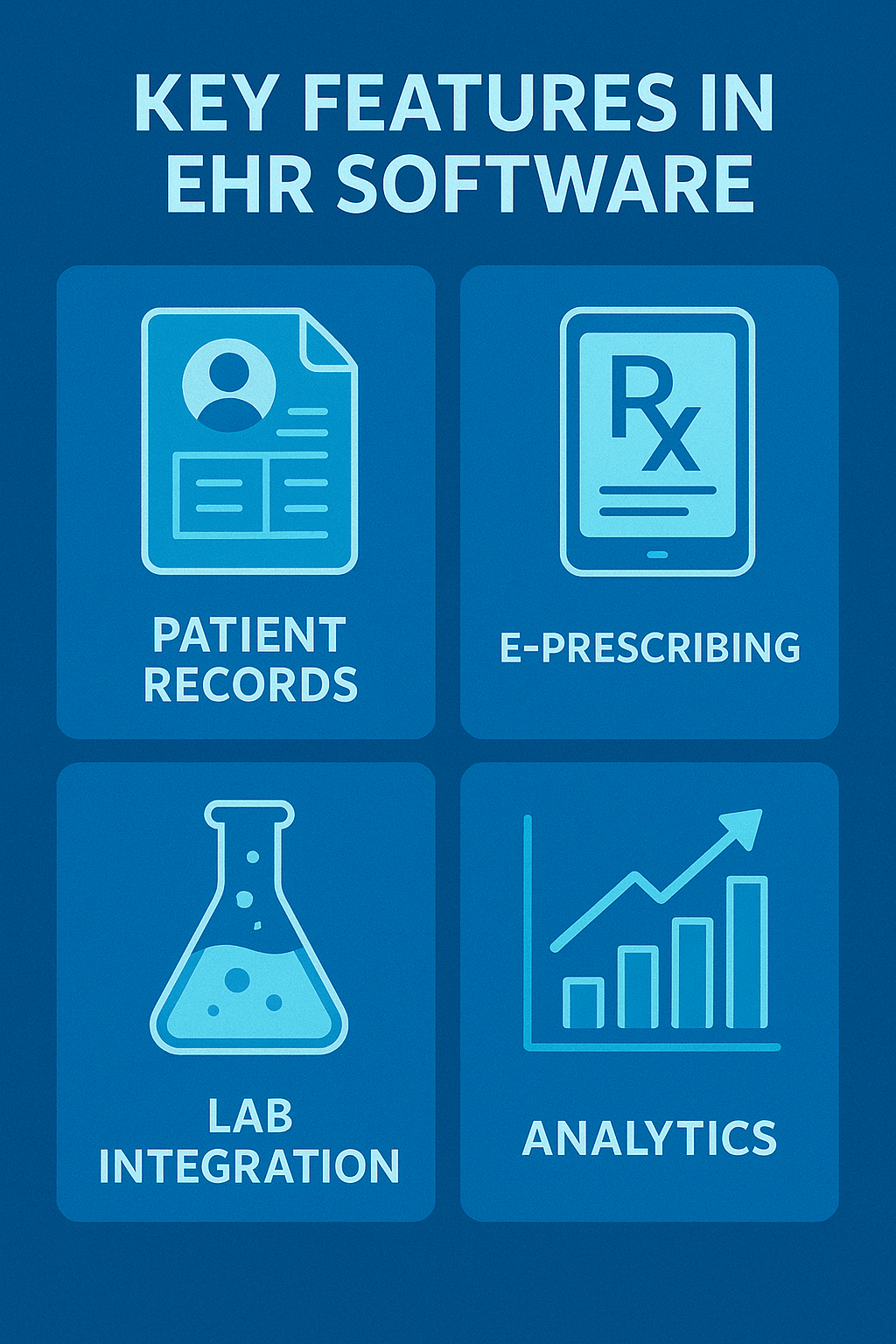
EHR Software Development: Key Features Should be integrated while development
Below, we outline the major features and capabilities one should expect in an EHR platform, with an eye on how each adds value to healthcare providers and patients.
-
Appointment Scheduling & Calendar
-
Patient Records & Demographics
-
Clinical Documentation (Notes & Charting)
-
Computerized Physician Order Entry (CPOE)
-
Results Management (Lab & Imaging Integration)
-
Medication Management
-
Clinical Decision Support
-
Billing & Coding Integration
-
Reporting & Analytics
-
Interoperability & Data Exchange
-
Patient Portal & Engagement
-
Security & User Access Controls
1. Appointment Scheduling & Calendar
Efficient scheduling is at the heart of practice operations. EHR software usually includes a calendar-based appointment management module that allows front-desk staff and clinicians to schedule patient visits, procedures, or follow-ups with ease.
Key capabilities include setting up provider calendars (with availability, time slots, and locations), patient self-scheduling (if a portal is available), and sending automated reminders to reduce no-shows.
A good scheduling feature will integrate with other parts of the EHR – for instance, linking appointments to patient records (so clicking an appointment pulls up that patient’s chart), and flagging any prerequisites (like insurance authorization or lab results needed before a visit).
Custom EHR development can further refine scheduling, such as enabling custom visit types, resource scheduling (for equipment or rooms), or waitlist management to fill canceled slots.
2. Patient Records & Demographics
At its core, an EHR contains comprehensive electronic patient charts. This feature stores all essential patient information – personal details and demographics (age, contact info, insurance), medical history, problem lists (diagnoses), allergies, immunization records, and more.
EHRs organize this data in a coherent way, often with a “summary” view for quick reference and detailed sections for each category. Clinicians should be able to easily review past visit notes, hospital discharge summaries, operative reports, etc., to understand a patient’s longitudinal health story.
A powerful search function to find specific entries (e.g. past MRI results or consultations) is also part of this feature. Ensuring data is well-structured (using standardized codes for diagnoses and procedures) is important for interoperability and analytics.
3. Clinical Documentation (Notes & Charting)
EHR systems provide tools for documenting patient encounters. This includes progress notes, history and physical (H&P) exams, procedure notes, etc. Modern EHRs often offer multiple input methods: structured templates, free-text typing, voice recognition dictation, or even smart forms that adjust based on inputs.
Features like auto-population (pulling in recent lab results or vital signs into the note) and templates by specialty help speed up documentation while maintaining quality. Custom EHRs might allow very specific templates or macros that align with a provider’s style of note-taking.
The documentation module should facilitate coding and billing as well – e.g., by linking the documented diagnoses and procedures to billing codes (ICD-10, CPT) to streamline charge capture.
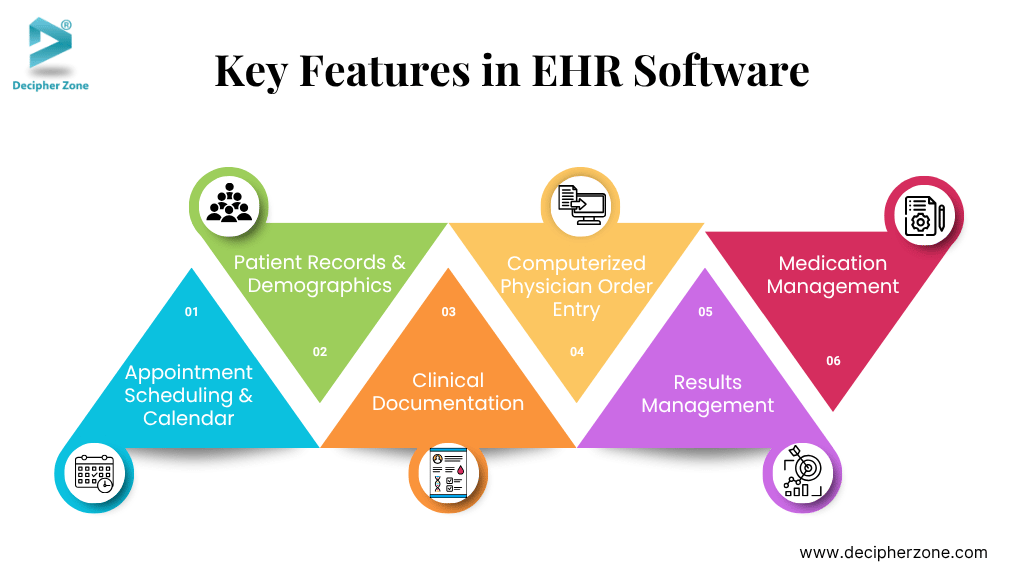
4. Computerized Physician Order Entry (CPOE)
This feature allows providers to order services electronically – such as laboratory tests, imaging studies (X-rays, MRI, etc.), medications (e-prescribing), and referrals. Instead of paper order forms or phone calls, a clinician enters orders into the EHR and they are transmitted to the relevant department or pharmacy.
CPOE reduces errors (no messy handwriting, and built-in checks can catch issues). A good EHR’s CPOE module includes decision support like alerting the prescriber to drug-allergy interactions, drug-drug interactions, or duplicate test orders.
E-Prescribing is a particularly impactful part: the EHR integrates with pharmacy networks so that prescriptions are sent directly to the patient’s pharmacy of choice, often with formulary checks (to choose medications covered by the patient’s insurance).
For custom systems, one might integrate specific formulary databases or add custom order sets (groups of orders for a certain scenario, like an admission order set).
5. Results Management (Lab & Imaging Integration)
An EHR isn’t complete without the ability to receive and display results from laboratories, imaging centers, and other diagnostic services. This feature fetches incoming data (lab test results, radiology reports, pathology reports) and attaches them to the correct patient record, often with alerts to the ordering provider.
Good EHRs present results in a user-friendly format – for example, trending lab values over time in a graph, or viewing a scanned X-ray image within the record. Integrating with PACS (Picture Archiving and Communication System) allows actual diagnostic images to be accessible.
A custom EHR solution can tailor how results are flagged (e.g., critical values generating immediate alerts), and allow providers to sign off on (acknowledge) results or forward them to other team members for follow-up. Quick access to historical results and the ability to compare them (e.g., previous blood tests or serial imaging) is crucial for quality care.
6. Medication Management
Beyond just prescribing, EHRs maintain an active medication list for each patient, including current medications, dosages, and start/stop dates. The system should track medication histories and support medication reconciliation (comparing a patient’s reported meds vs. what’s in their record to ensure accuracy at transitions of care).
Features like drug databases, interaction checkers, and formulary info assist providers in managing medications safely. Some EHRs also integrate with pharmacy fulfillment data (to see if patients picked up their prescriptions) or with medication adherence tools.
"We looked into building an EHR system last year. The biggest challenge was complying with HL7/FHIR standards while keeping the UX simple. Most startups fail not on tech, but on understanding clinician workflows."
– Reddit user on r/healthIT
7. Clinical Decision Support
Many EHRs incorporate decision support systems to aid providers in making evidence-based decisions. This can range from simple alerts (“Patient due for a flu vaccine” or “Recent lab result is abnormal”) to more advanced tools like care guidelines and diagnostic suggestions. For example, an EHR might notify a physician if a patient’s lab values meet criteria for a condition or if a prescribed dose is outside the normal range.
Order sets and care plans embedded in the EHR can guide providers through best practices for common conditions. The goal is to leverage the digital platform to improve care quality and consistency. It’s important that these alerts are well-tuned (to avoid alert fatigue).
A custom EHR can allow an organization to configure decision rules according to its protocols or use specialized calculators and risk scores relevant to its patient population.
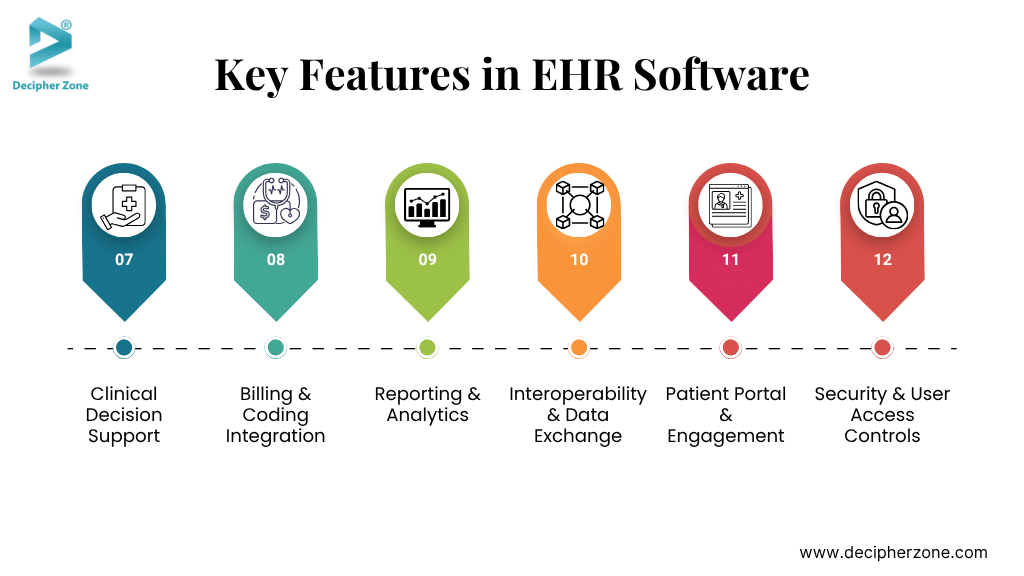
8. Billing & Coding Integration
Since clinical care and billing are intertwined, EHR software usually includes or integrates with a practice management / billing system.
Key features include capturing charges as part of documentation (so providers can select billable codes during their workflow), verifying insurance eligibility, and generating billing claims (to send to payers).
Financial dashboards or reports might be included to monitor revenue cycle metrics. In a custom setup, the billing component can be tailored to local requirements or specific specialties (for instance, a behavioral health clinic might need support for session-based billing and authorization tracking).
9. Reporting & Analytics
EHRs hold a treasure trove of data that can be used for analytics and quality reporting. Built-in reporting tools allow administrators or clinicians to run queries – for example, list all diabetic patients who haven’t had an eye exam this year, or track clinic-wide outcome measures.
Many systems provide dashboards with key performance indicators (KPIs) like patient wait times, provider productivity, or population health metrics. Custom EHR solutions can create bespoke reports and integrate data visualization tailored to the organization’s strategic goals.
Reporting is also important for regulatory compliance (e.g., generating reports for quality programs or clinical trials).
10. Interoperability & Data Exchange
A hallmark of true EHR systems is interoperability – the ability to share and exchange health information with other entities. Core interoperability features include generating and consuming standardized data formats such as HL7 messages or FHIR APIs.
This allows an EHR to send summary of care records to another provider, query a Health Information Exchange (HIE) for patient records from outside organizations, or import patient data from wearable devices and remote monitors. EHRs may also support Direct Messaging, a secure email-like system for exchanging clinical documents.
In the U.S., modern EHRs meet certification criteria that require providing patients with electronic access (like downloading their records or using third-party health apps via FHIR).
Custom EHR development projects often prioritize the specific integration points needed (e.g., connecting with a national immunization registry, or integrating with a telehealth platform’s data). Smooth data exchange is key to coordinated care, so this feature cannot be overlooked.
11. Patient Portal & Engagement
Most EHRs offer a patient-facing portal or app as part of the package. This portal allows patients to securely log in and perform various actions: view their test results and visit summaries, schedule appointments or request refills, message their providers, fill out intake forms, and make payments, among others.
Patient engagement features like portals are increasingly important – they empower patients to be involved in their care and improve satisfaction. A custom EHR might integrate a portal deeply with clinic workflows (for example, patient-submitted data from the portal flows right into the EHR for review).
Additionally, features like telehealth (video visits) or remote patient monitoring data integration can be considered part of patient engagement in today’s digital health landscape.
12. Security & User Access Controls
Given the sensitive nature of health data, a robust EHR must have strong security features. This includes role-based access (controlling who can see or edit certain information), audit trails logging every access or change to a record, and data encryption (both in the database and for data in transit).
Features like automatic log-off after inactivity, multi-factor authentication, and privacy filtering (e.g., break-the-glass protocols for confidential records) are also common.
While these may not be “visible” features in marketing, they are absolutely essential and often built into the architecture of any reputable EHR system. We will discuss this more in the compliance section, but it’s worth noting here as a feature checklist item.
Read: Healthcare Digitalization Trends
EHR Software Development: Why UI/UX Matters?
Unlike many other industries, in healthcare the stakes are literally life and death. A confusing interface that buries critical information or causes delays isn’t just an annoyance; it can impact patient care.
Poor EHR usability has been linked to physician burnout and safety issues. Research has shown that there is a strong correlation between perceived EHR usability and provider burnout levels.
For instance, a well-known study in the Mayo Clinic Proceedings found that on a standardized usability scale (SUS), physicians rated EHRs with an “F” grade on average, and that for each 1-point improvement in usability, the odds of physician burnout dropped by 3%. That’s a significant impact – it underscores that improving the EHR interface isn’t just a nice-to-have; it directly affects providers’ well-being and their ability to care for patients effectively.
We also know from human factors research that when users are overwhelmed or systems are counter-intuitive, mistakes can happen. In healthcare, that might mean a medication dose is entered incorrectly or a critical lab result is overlooked, potentially causing patient harm.
For example, if an alert is poorly designed or fires too often (false alarms), clinicians might start ignoring them (“alert fatigue”), possibly missing a real warning about, say, a dangerous drug interaction. Good UX design in an EHR will prioritize information clearly and reduce cognitive load on the user, helping them make the right decisions quickly.
EHR Software Development: Key Principles of UI/UX Design
Here are the list of UI/UX design priniciples.
-
User-Centered Design
-
Simplicity and Clarity
-
Visual Prioritization
-
Workflow Integration
-
Speed and Responsiveness
-
Error Prevention and Handling
-
Adaptability and Customization
-
Training and Onboarding
-
Mobile and Responsive Design
1. User-Centered Design
The design process should involve actual end-users (doctors, nurses, etc.) from the beginning. This means conducting workflow analysis, interviews, usability testing with prototypes, and iterative improvement based on feedback. Developers and designers have to remember that clinicians often work under intense time pressure.
Observing a nurse triage patients or a physician during a busy clinic can reveal pain points that you’d never catch otherwise. By tailoring the UI to fit their mental models and workflows, you end up with a product that feels natural.
For instance, if a physician says, “When I open a patient chart, the first thing I need to see is the latest progress note and lab results,” then the UI should reflect that, perhaps by having a dashboard or summary view with those elements prominent.
2. Simplicity and Clarity
Medical data is complex, but the presentation should aim for simplicity. This doesn’t mean dumbing it down or omitting details; rather, it means organizing information in a clear hierarchy and avoiding clutter. Use whitespace and grouping to make screens scannable.
Standardize on terminology and icons so users don’t have to guess (“Lab Results” should always be called that, not sometimes “Investigations”, etc., unless adapting to local jargon consistently). Consistency in layout across modules helps users form habits (for example, the “Save” or “Sign” button should be in a consistent location).
A common complaint about some EHRs is the number of clicks needed to do things. A rule of thumb is the “three-click rule” – try to ensure users can reach what they need in three clicks or less whenever possible. If a nurse has to click through 10 screens to record a routine vaccination, that’s a UX fail.
3. Visual Prioritization
Not all information on a given screen is equally important at that moment. Good UI uses visual cues (like font size, color highlights, bold text, or icons) to draw attention to critical data.
For example, abnormal lab values could be shown in red or with a warning icon, whereas normal values are in regular text. In an inbox of patient messages, maybe urgent messages (like a patient reporting severe symptoms) are flagged to stand out.
However, careful with color usage – designs should be accessible (consider color-blind users, so not relying solely on color differences). Also, don’t overdo it: if everything is highlighted, nothing stands out.
4. Workflow Integration
The UI should mirror clinical workflows. That means if a doctor typically reviews a patient’s history, then current meds, then writes a note and orders tests, the EHR should make that sequence logical and smooth. Features like “single-screen workflows” are appreciated – for example, some EHRs allow viewing relevant past data right alongside the order entry screen, so you don’t have to navigate away to check something.
Another aspect is reducing context switching – if a physician has to jump between many modules for one task, it’s taxing. Contextual design (showing everything needed for the task at hand in one place) is ideal.
For instance, a discharge summary workflow could present the final diagnosis, follow-up instructions, medication changes, and discharge prescriptions in a guided sequence so nothing is forgotten and it’s all completed together.
✅ Ready to build your HIPAA-compliant EHR system? Talk to our experts at Decipher Zone
5. Speed and Responsiveness
UX is not just look-and-feel; performance is a UX issue too. An interface that lags or takes several seconds to load each page will frustrate users no matter how pretty it looks. Clinicians often note that waiting on an EHR (like staring at a loading spinner) is a major frustration.
Optimizing the software for quick response – through both front-end and back-end performance improvements – pays dividends in user satisfaction.
This includes things like using progressive loading (load essential info first, then less critical details), avoiding blocking operations on the UI thread, and pre-fetching data if possible (for example, if you know the doctor will likely click “Labs” next, maybe pre-load lab results in the background while they are reading notes).
6. Error Prevention and Handling
A well-designed UI helps prevent user errors, and if errors occur (like missing data or system errors), it communicates clearly. Use constraints and validation to prevent invalid inputs (e.g., don’t allow letters in a numeric field, or give a warning if a entered dose is way out of range).
If a user tries to prescribe a medication the patient is allergic to, a meaningful alert should pop up – and then, importantly, allow an appropriate override if clinically justified (with a reason). When users do make mistakes or the system encounters an issue, error messages should be informative (no cryptic codes) and guide the user on what to do next (“Please select a patient before printing” instead of just “Error 402”).
Also, an “undo” or edit ability is great to have for non-permanent actions, which can reduce fear of using the system (e.g., if I accidentally close a note I was writing, can I retrieve it? The system could autosave drafts).
7. Adaptability and Customization
While consistency is key, providing some customization options can significantly improve UX for different users. For example, some doctors might want to see data in a flowsheet (tabular format), others might prefer graphs – an EHR can offer both views.
Allowing users to set preferences (like default screen on login, font size, dark mode for working at night, or quick-action shortcuts) can make the system more comfortable.
Clinicians often develop their own workflow “style,” so accommodating that within reason (without compromising overall usability) is beneficial. However, the baseline design should be solid – customization is a bonus, not a crutch to fix poor design.
8. Training and Onboarding
Even the best-designed EHR will have a learning curve (there’s just a lot to know). The UX extends to how new users get acquainted. Providing an intuitive navigation structure (so exploring is self-guided) and possibly built-in help or tooltips can reduce training burden.
Some systems now have interactive tutorials or “coach marks” that highlight what’s new after an update. Because healthcare staff turnover can be high and they might not always get extensive training time, making the system as discoverable as possible is a plus. If someone can figure out the basics without a manual, that’s a UX win.
9. Mobile and Responsive Design
Increasingly, healthcare providers want to use tablets or even smartphones for certain tasks (e.g., a doctor doing rounds with a tablet, or a home health nurse using a mobile app). Ensuring the EHR interface (or a companion app) is responsive and mobile-friendly is important.
This might involve designing simplified views for mobile that focus on just the key info and input needs for on-the-go use. It’s part of UX to consider the different contexts of use – e.g., desktop in an office vs. tablet at bedside – and optimize for each.
Read: Virtual Hospital Software Development
EHR Software Development Cost Breakdown
In this section, we’ll break down the typical components of EHR development cost and provide some insights into how each factor contributes to the overall budget. By understanding the cost structure, stakeholders can plan better and make informed decisions on budgeting and resource allocation.
-
Software Development Costs
-
Hardware and Infrastructure
-
Licensing and Third-Party Services
-
Data Migration
-
Integration Costs
-
Testing and Validation
-
Training and Onboarding
-
Deployment and Configuration
-
Support and Maintenance (Ongoing Costs)
1. Software Development Costs
This is the core cost of coding and creating the software. It includes the salaries (or contract fees) for software engineers, UI/UX designers, testers (QA), business analysts, and project managers involved in the project. If you’re outsourcing development to a software company, this often comes as a project quote. A custom EHR can easily require a team of 5-15 people (or more) working for many months or years, depending on complexity.
For instance, one estimate suggests that a custom EHR solution could cost $50,000 to $250,000+ just in development, depending on features and complexity. This cost scales up with the size of the project: more features, more integration, more customizations = more development hours.
Using established frameworks or open source components can reduce some cost, but careful with licensing if using third-party libraries. Additionally, building to meet compliance (security features, etc.) might add to dev time compared to a simple app.

2. Hardware and Infrastructure
Even if the EHR software itself is custom, it needs to run on something. Costs here include servers (or cloud infrastructure), networking equipment, backup solutions, etc. If an on-premises deployment is planned, the organization might need to purchase new server hardware and possibly upgrade network bandwidth (especially if many heavy imaging files or many concurrent users will stress the network).
For on-prem, consider load balancers, database servers (with redundancy), storage arrays for data and backups, etc. According to some breakdowns, hardware costs for EHR can range from a few thousand to tens of thousands of dollars – e.g., $1,000-$10,000 per device (like a new computer or tablet for each provider) and servers which could be $10k-$50k depending on size.
In a cloud or SaaS model, instead of upfront hardware, you’d budget for ongoing cloud hosting costs, which might be monthly based on usage (but over a multi-year period, that can sum up to similar amounts).
3. Licensing and Third-Party Services
If the project uses any third-party components, there may be licensing fees. For example, maybe you integrate a commercial drug database for medication decision support, or a medical speech-to-text engine for dictation those might have license costs per year or per user.
Similarly, if using an interface engine or integration platform that’s commercial, factor that in. If the software will connect to certain networks (like e-prescribing networks or claims clearinghouses), there might be subscription fees for those services. For an open-source approach, licensing cost can be near zero, but one must then account for more development effort to build those capabilities in-house.
4. Data Migration
As mentioned in challenges, migrating data from legacy systems is a project of its own. Often, organizations underestimate this cost. Data migration involves writing scripts, mapping data fields, testing migrated data, and sometimes manual data entry/clean-up. If legacy data is voluminous and spread across multiple systems (say an old EMR, a separate billing system, etc.), this can take many developer and analyst hours.
Some experts estimate data migration can cost tens of thousands of dollars for a mid-sized clinic migration. For example, engaging a data migration specialist or service could run $20,000-$50,000 depending on data complexity.
The cost goes up if many custom mappings or if data is unstructured (like scanning a bunch of paper records into the system – that involves labor and scanning equipment).
📅 Book a free consultation to assess your existing workflows and infrastructure.
5. Integration Costs
Building interfaces to other systems (labs, hospitals, devices, etc.) can also add notable cost. Each integration might require custom development and testing with the partner system. If using a third-party integration engine, there’s the tool cost and then the labor to configure it. According to one guide, integrating an EHR with other software can significantly increase budget needs.
Let’s say connecting to a lab information system takes a developer a month of work – that’s a cost to factor. Multiply by multiple integrations (pharmacy, lab, radiology, insurance, health information exchange) and it adds up.
Therefore, integration might be a line item of $X per interface. Some vendors charge, for example, $5,000-$10,000 per custom interface developed. In custom development, it’s just part of dev hours, but should be accounted for explicitly (because it can be time-consuming).
6. Testing and Validation
EHRs require extensive testing – not just standard software QA, but also clinical validation. You’ll likely do unit testing, integration testing, performance testing, and user acceptance testing. If following any regulatory guidelines (like for FDA class software, or ONC certification testing), that might involve specific test scripts and even hiring external auditors or testers.
Testing is labor-intensive and thus has a cost in personnel time. Some budgets allocate a substantial percentage (like 20-30%) of development time to testing phases. It’s money well spent to avoid dangerous bugs in production.

7. Training and Onboarding
When the software is ready to deploy, training the staff is a significant cost. This could include developing training materials (manuals, videos), conducting training sessions (paying trainers, or compensating staff for training time), and possibly running a mock clinic or parallel run to practice. Some clinics also use “super-users” (staff who get extra training and then help others), which might involve stipends or dedicated time.
Training costs can vary – some estimates for small practices are a few thousand dollars, whereas for a hospital it can be tens or hundreds of thousands, especially if backfilling positions while staff attend training.
For budgeting, one might say, e.g., $1,000-$5,000 per staff member in training costs when factoring their time and materials. In addition, you might consider the lost productivity during the learning curve as an indirect cost (often seen in the first few weeks after go-live).
"A top-tier EHR implementation can easily cross $100,000 to $500,000 depending on scope. The true cost often lies in change management, workflow disruption, and long-term support. It's not just about the software — it's about reengineering how your clinic operates."
– Insightful answer on Quora
This quote perfectly captures what many vendors overlook — the hidden costs of change. That’s why Decipher Zone recommends a **phased rollout and post-deployment training** during any custom EHR development engagement.
8. Deployment and Configuration
Setting up the production environment, configuring the EHR (e.g., creating user accounts, setting permissions, customizing templates, setting up forms, etc.) is another slice of work. Sometimes this is done by the implementation team rather than devs, but it’s still resource time.
If you are rolling out to multiple sites, travel costs might occur for trainers or IT staff. Configuration can also include customizing the system for particular specialties or departments (e.g., building a custom template for ophthalmology exams). All this usually happens in the run-up to go-live and can require significant overtime or consulting support.
9. Support and Maintenance (Ongoing Costs)
Often overlooked in initial budgeting is the post-launch maintenance. After the EHR is live, you’ll need ongoing technical support, future upgrades, bug fixes, and new feature development as needs evolve or regulations change. It’s common to budget an annual maintenance cost of around 15-20% of the initial implementation cost for software systems.
For example, if your EHR cost $300k to develop and implement, expect perhaps $45k-$60k per year in maintenance (this could cover a support developer or two, cloud hosting fees, minor enhancements, etc.). Maintenance includes server costs, software license renewals (if any), ongoing security updates, and so forth.
Planning for these costs ensures the system remains secure and up-to-date. In some cases, if the custom EHR is large, an in-house IT team or a contract with the development firm for support will be needed – which is a recurring expense.
Read: Dental Software Development
EHR Software Development: Key Factors Influencing Cost
As a summary, let’s highlight the major factors that cause EHR project costs to fluctuate:
-
Size and Complexity of the Organization
-
Customization Needs
-
Integration Requirements
-
Regulatory Environment
-
Timeline
-
Vendor vs In-house Development
-
Scope Creep
1. Size and Complexity of the Organization
A larger hospital system will have more users, more departments with unique needs, and more data, leading to higher costs. More users also mean more hardware and training costs. Complexity in terms of multiple specialties or service lines adds cost because you effectively are building multiple tailored workflows in one EHR.
2. Customization Needs
If the EHR must be heavily customized or built from scratch to meet specific requirements, the development time goes up. Custom features (like a specialized oncology module or research data capture functions) will increase costs, though they may be essential for meeting goals.
3. Integration Requirements
Each third-party integration (labs, imaging centers, device feeds, etc.) will add to the budget, both initially and for maintenance (since interfaces may break when either side updates).

4. Regulatory Environment
Operating in regions with strong data protection laws (e.g., GDPR) might require more investment in compliance features and documentation. Participating in government programs might necessitate certification (with its associated costs).
5. Timeline
If a quick turnaround is needed, you might need to hire more developers or pay overtime, or accept higher risk (which might lead to issues that need fixing later). Rushed implementations often incur higher costs due to inefficiencies, need for rework, or hiring additional temporary help. Conversely, a more extended timeline might spread costs out, but prolonged projects can also accumulate cost if not managed.
6. Vendor vs In-house Development
If engaging a vendor or development partner, their pricing models (fixed vs time-and-material) will affect cost clarity. In-house development might save some money but could take longer if the team is small, plus you carry the ongoing HR costs. Some organizations opt for a hybrid: buy a base product and then invest in customizing it – that splits cost between license fees and dev fees.
7. Scope Creep
It’s almost inevitable that new ideas or needs surface during the project. Uncontrolled scope creep can inflate costs significantly. Strong project governance is needed to evaluate change requests and possibly defer some to a “Phase 2” after initial go-live.
To give a rough idea of some cost ranges (combining many of the above components):
-
For a small practice (1-5 providers), implementing a basic EHR might cost anywhere from $20,000 to $65,000 overall (this might involve using a simpler system or limited customization).
-
For a mid-sized clinic or practice with some customization, costs might be in the range of $65,000 to $200,000.
-
For a large hospital or multi-site health system, a custom or highly customized EHR could run $200,000 to $650,000 or more. In fact, some well-known hospital EHR implementations (with commercial vendors) have reached tens of millions of dollars when accounting for all factors – albeit those are massive scales.
Read: Healthcare Inventory Management Software Development
EHR Software Development: Top 10 Business Benefits
Let’s explore some of the key strategic advantages of a well-implemented EHR system:
-
Operational Efficiency and Cost Savings
-
Enhanced Revenue Cycle Management
-
Better Quality of Care (Leading to Financial Incentives)
-
Improved Patient Satisfaction and Retention
-
Data-Driven Decision Making (Business Intelligence)
-
Scalability and Growth Enablement
-
Compliance and Risk Management Benefits
-
Competitive Advantage & Innovation
-
Long-term Cost Avoidance
-
Better Provider Satisfaction and Retention
1. Operational Efficiency and Cost Savings
One of the clearest benefits of digitizing and streamlining workflows with an EHR is improved efficiency. Tasks that used to be time-consuming – hunting for paper charts, duplicating tests because prior results weren’t available, manually entering billing codes – are greatly reduced. With an EHR, staff can handle larger volumes of patients or spend more time on value-adding activities rather than paperwork.
Over time, this efficiency translates into cost savings for the organization. For example, a McKinsey analysis found that when done right, EHR implementation can lead to about a 5–10% reduction in operational costs through increased efficiency and automation.
Savings come from areas like reduced transcription costs (if doctors directly enter notes or use voice recognition), less overtime for administrative staff, and lower paper handling expenses.
Additionally, electronic processes (like e-prescribing or electronic referrals) can shorten service delivery times (patients get their meds or appointments faster), which improves throughput and potentially revenue.
2. Enhanced Revenue Cycle Management
EHRs often integrate with or include billing systems, which can notably improve revenue capture and reduce billing errors. With proper documentation templates and coding support, physicians are more likely to capture the full extent of services provided (no more missed charges due to illegible notes or forgotten procedures).
The system can prompt for coding specifics and ensure that billing codes are backed by documentation, thus reducing denied claims. Also, automation of insurance eligibility checks and claim submissions speeds up reimbursement. Some studies have shown that an EHR can increase revenues by enabling more accurate coding (upcoding when appropriate because documentation supports higher complexity) and by reducing lost charges.
In fact, a cost-benefit analysis in primary care predicted a net financial benefit of about $86,400 per provider over 5 years post-EHR adoption, largely from improved charge capture and reduced drug costs and test utilization. That’s a substantial ROI, meaning the EHR can pay for itself over time.
Industry Insight:
“EHR implementation not only improves documentation accuracy but also boosts operational efficiency — especially when integrated with AI-based clinical decision support.”
3. Better Quality of Care (Leading to Financial Incentives)
EHRs contribute to improved patient outcomes by facilitating evidence-based medicine and preventive care reminders. From a business perspective, better care quality can mean better performance on quality metrics, which in many healthcare systems ties into financial incentives.
For example, in value-based care models or pay-for-performance programs, meeting certain clinical quality benchmarks can yield bonus payments or shared savings. An EHR makes it easier to track those metrics (like controlling diabetic patients’ blood sugar or ensuring patients receive immunizations) and to implement interventions (like alerts for overdue screenings).
Moreover, preventing errors and adverse events through decision support is not only a patient safety benefit but also a financial one – it avoids costs associated with treating preventable complications.
For instance, by catching medication conflicts or allergies, the system helps avoid adverse drug events, which can be expensive. A study projected that EHR decision support could cut 34% of adverse drug events and reduce associated costs accordingly.
Avoiding such events saves on liability and improves hospital performance metrics (like lowering readmission rates, which Medicare and others pay attention to).
4. Improved Patient Satisfaction and Retention
Happy patients are good for business. EHR features like a patient portal, online scheduling, and electronic communication improve the patient experience. Patients appreciate being able to get lab results quickly, request refills without waiting on hold, or message their doctor with follow-up questions.
A smoother experience can increase patient loyalty to the practice and reduce churn. It might also attract new patients (for instance, tech-savvy individuals may prefer providers who offer modern conveniences). In competitive healthcare markets, offering such digital services is becoming a differentiator.
High patient satisfaction scores can also impact reimbursement in certain healthcare settings (like HCAHPS scores in hospitals influencing Medicare payments). So, from a strategic viewpoint, an EHR that enhances patient engagement contributes to the practice’s reputation and financial health.
💡 Need EHR for your specialty practice? Let’s build it from the ground up—tailored to your needs.
5. Data-Driven Decision Making (Business Intelligence)
EHRs centralize a wealth of data that can be harnessed for strategic decisions. Administrators and practice owners can run reports to analyze trends – e.g., patient volume by service, no-show rates, common diagnoses, resource utilization, etc.
This kind of business intelligence helps in planning and optimizing operations. Perhaps the data shows that certain clinic hours are underutilized while others are overbooked – you could adjust staffing or scheduling templates accordingly. Or analyzing referral patterns might spur decisions to add a service line that many patients are being referred out for.
On a larger scale, health systems use EHR data to identify opportunities for improving care pathways that also save money (like reducing unnecessary tests). In essence, an EHR transforms raw health records into actionable insights for management when paired with good analytics tools.
6. Scalability and Growth Enablement
For health tech startups or growing provider networks, having a robust EHR infrastructure in place enables expansion. You can onboard new providers or clinics more easily when you have a standardized electronic system – their data can integrate into the central database, and they can adhere to the same workflows.
If you’re expanding services (say telemedicine or remote monitoring programs), a modern EHR likely has modules or API capabilities to incorporate those. This scalability means the organization can pursue growth opportunities (mergers, acquisitions of practices, adding new specialties) without being held back by disjointed or archaic record systems.
In a way, the EHR becomes a platform on which you can build new digital health offerings or integrate future innovations (like AI diagnostic tools) – positioning the business at the forefront of healthcare technology.

7. Compliance and Risk Management Benefits
Strategically, using an EHR helps with regulatory compliance (as we covered) which indirectly protects the business from legal and financial risks. Complete and legible records reduce malpractice risk (many malpractice cases hinge on missing or illegible documentation).
Audit trails and controlled access protect against unauthorized data breaches, which could otherwise result in heavy HIPAA fines. Also, with an EHR it’s easier to demonstrate compliance during audits (be it for accreditation, insurance, or government programs) by quickly producing required reports.
This risk mitigation is a bit intangible but extremely valuable – one breach or compliance issue can cost a fortune and damage the organization’s reputation. So, in business terms, an EHR is part of a robust risk management strategy, providing peace of mind that you’re meeting obligations and can prove it when needed.
8. Competitive Advantage & Innovation
In the healthcare market, those who leverage technology effectively often stand out. A custom EHR can be a competitive differentiator, especially if it’s tailored to a niche or provides capabilities others lack.
For example, imagine a specialty practice that has built in a telehealth workflow or specialized decision support for their field – they might attract patients and referring physicians because they deliver more seamless, informed care. For health tech companies, owning a unique EHR solution could be part of their intellectual property and market offering.
Additionally, having control over your EHR allows you to innovate faster. Want to implement a new care model or pilot a population health program? You can adapt your software to support it.
We saw during the COVID-19 pandemic how organizations with flexible IT could quickly set up vaccine clinics or remote patient monitoring, whereas those on rigid systems struggled. Being able to adapt can be a competitive edge.
9. Long-term Cost Avoidance
While there’s an upfront cost to implementing an EHR, in the long run it can help avoid or reduce various costs. For instance, paper record management (storage, staff time to pull files) – going digital removes those.
It also helps avoid costs associated with medical errors and duplication (which, beyond patient harm, have financial costs like additional treatments, extra hospital days, etc.).
In a practice, efficient billing and fewer denied claims mean more steady cash flow and less effort chasing payments. A well-implemented EHR can also improve coding compliance, reducing the risk of audits or penalties from payers for incorrect coding.
10. Better Provider Satisfaction and Retention
From a business standpoint, keeping your doctors and nurses happy is crucial – recruiting and replacing clinical staff is expensive and difficult. A good EHR (especially one customized to reduce annoyances) can improve provider work-life balance.
For instance, if the EHR reduces after-hours charting by making documentation more efficient, providers are less burnt out and more likely to stay with the organization.
In contrast, we’ve seen cases where a terrible EHR led to physicians quitting or even organizations reversing implementation. So, indirectly, a solid EHR contributes to workforce stability, which is a huge asset. It’s easier to execute on business strategy when your clinical team is not overburdened by tech woes.
Read: On-demand Medicine Delivery App
EHR Software Development: Case Study Snippets
Let’s look at a brief case study example from Decipher Zone’s experience in healthcare software projects. These snippets highlight practical outcomes and lessons from developing and implementing tailored EHR/EMR solutions.
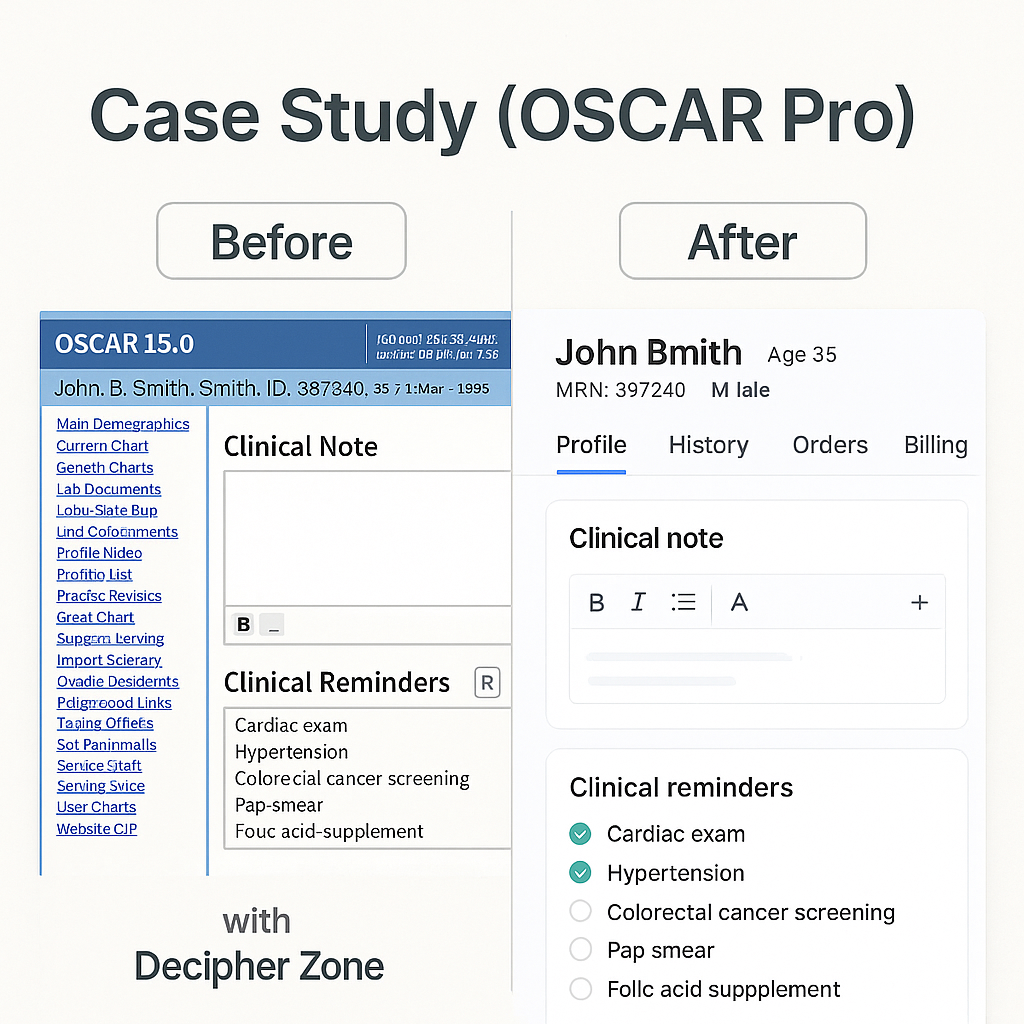
Case Study: OSCAR Pro EMR Modernization
Decipher Zone Technologies collaborated with OSCAR Pro, a leading provider of open-source EMR solutions in Canada, to enhance and modernize their electronic medical record platform. The project’s goal was to streamline physician workflows and improve the overall user experience for hundreds of clinicians using OSCAR Pro across primary care clinics.
Project Overview
OSCAR Pro’s existing EMR system had a solid user base but needed an upgrade in terms of performance, UI/UX, and some added functionalities (like better scheduling and telehealth integration) to meet the evolving needs of clinics. Decipher Zone’s team engaged to refactor and extend the platform while ensuring minimal disruption to existing users.
Technologies & Approach
We employed a robust Java-based tech stack: Spring Boot and Hibernate on the backend for scalability and maintainability, and a refreshed frontend built with modern web technologies. The database (MySQL) was optimized, and legacy code was carefully refactored module by module.
We also integrated Apache Tomcat for the web server and utilized tools like Jenkins for continuous integration and deployment. Throughout development, we worked closely with actual OSCAR Pro users (doctors and clinic staff) to get feedback on UI prototypes and ensure the enhancements were aligned with their workflows.
Outcomes
The revamped OSCAR Pro EMR was delivered as a secure, efficient, and scalable solution. Clinics reported that the system felt more responsive – average page load times were significantly reduced. The new user interface was cleaner and more intuitive, resulting in less time spent on training new staff.
Notably, the appointment scheduling module we redesigned allowed clinics to handle increased patient volume with the same staff, effectively boosting productivity. Physicians praised the new features like quick-access dashboards and the integrated telehealth module (especially timely during the COVID-19 pandemic when virtual visits spiked).
From a business standpoint, OSCAR Pro strengthened its position in the market; the improvements attracted several new clinics to choose OSCAR Pro as their EMR provider. The project demonstrated how custom modernization of an EMR can extend the life of a platform and add substantial value for users, without them having to switch systems.
"Oscar EMR is great once you get the hang of it, but the initial learning curve was steep. The interface is functional but dated, and we had to invest in external training for our admin staff."
– Verified user on G2
Many clinics face similar friction when using off-the-shelf solutions. With custom EHR systems, you can build **role-specific UI flows** that match your internal processes — reducing reliance on third-party training and improving adoption.
Decipher Zone’s Role
Throughout this project, Decipher Zone leveraged its expertise in custom healthcare development to ensure that enhancements met high standards of privacy (HIPAA/PIPEDA compliance) and reliability. We also provided ongoing support post-launch to quickly address any live issues. The successful deployment with minimal downtime built trust with the client and end-users.
In the words of an OSCAR Pro representative: “Decipher Zone’s tailored approach and expertise in cutting-edge technologies helped OSCAR Pro deliver an EMR solution that is secure, efficient, and scalable”. This endorsement highlights our commitment to EHR excellence and collaboration with domain experts.
Conclusion
In conclusion, Electronic Health Record software development is a transformative undertaking that can elevate a healthcare organization’s capabilities, efficiency, and quality of care.
A well-crafted EHR system becomes the digital backbone of a medical practice or hospital – streamlining everything from scheduling appointments to documenting encounters, ordering tests, prescribing medications, billing, and analyzing health outcomes.
Is your healthcare organization ready to harness the full potential of a custom EHR solution? Whether you’re looking to develop a new Electronic Health Record system from scratch, tailor an existing platform to better fit your needs, or integrate cutting-edge features like telehealth and AI analytics – Decipher Zone is here to help turn your vision into reality.

As a leading custom software development company with substantial experience in EHR and medical software projects, Decipher Zone brings the perfect blend of technical expertise and healthcare understanding to the table.
We pride ourselves on delivering people-first, high-quality solutions that truly make a difference in clinical practice and healthcare business outcomes. Our team has a track record of building secure, user-friendly, and compliant software – all while keeping your goals and end-users at the forefront.
Read: Impact of AI on the Healthcare Industry in 2025
Let’s collaborate to transform your healthcare IT:
-
Request a Consultation: Reach out to us for a free, no-obligation consultation about your EHR or healthcare software needs. We’ll listen to your challenges and ideas, share our insights, and explore how a custom solution could provide the results you’re looking for.
-
Explore Your Options: Not sure where to start? Our experts can help analyze your current systems and workflows, and then recommend a tailored roadmap – be it developing a new module, integrating systems, or a full EHR implementation plan. We’ll help you weigh the build vs. buy decision objectively with your specific context in mind.
-
Get a Proposal: If you have a project in mind, we’d be happy to put together a detailed proposal, including scope, timeline, and cost estimates. Transparency and collaboration are hallmarks of how we work – you’ll always know what to expect.
-
See Our Work in Action: We can arrange a demo of relevant case studies or even a prototype to give you a tangible sense of what Decipher Zone can deliver. For instance, if you’re curious about a particular feature (say, an intuitive dashboard or a telemedicine plugin), we can showcase examples of our past work.
Don’t let outdated systems or generic software hold back your healthcare practice. Empower your team with a custom EHR that is built around how you work, not the other way around. The efficiencies gained, errors reduced, and improvements in care coordination will speak for themselves – and your patients and staff will thank you.
Contact Decipher Zone today to start the conversation about your EHR software development project. Together, we can develop a flagship solution that sets you apart as a technology-enabled healthcare leader.
🙋♂️ Frequently Asked Questions
What’s the difference between EMR and EHR?
EMR is digital records for one practice, while EHR is sharable across providers, offering a more comprehensive patient view.
Is it mandatory to follow HIPAA for EHR development?
Yes, if your software handles patient data in the US, HIPAA compliance is legally required.
How long does it take to develop an EHR system?
Typically, 6–12 months, depending on complexity, integrations, and team size.
Can EHR software integrate with telemedicine platforms?
Absolutely. APIs allow EHRs to sync with video consultation tools, prescription services, and appointment systems.
**Disclaimer**: Some images used in this article have been generated with the assistance of AI

