In this comprehensive guide, we’ll explore the top 10 types of healthcare software in 2025. We’ll cover everything from patient-facing mobile apps to enterprise hospital systems, highlighting how each solves real problems in healthcare. You’ll learn what each software type does, see practical examples and use cases, and get insights on current trends (especially in the U.S. and EU). Our aim is to answer your questions and help you make informed decisions – whether it’s choosing the right system for your clinic or identifying opportunities for new healthcare software development.
Technology is transforming healthcare in 2025. From the smartphone in a patient’s hand to the sophisticated systems running entire hospitals, healthcare software now touches every aspect of care delivery.
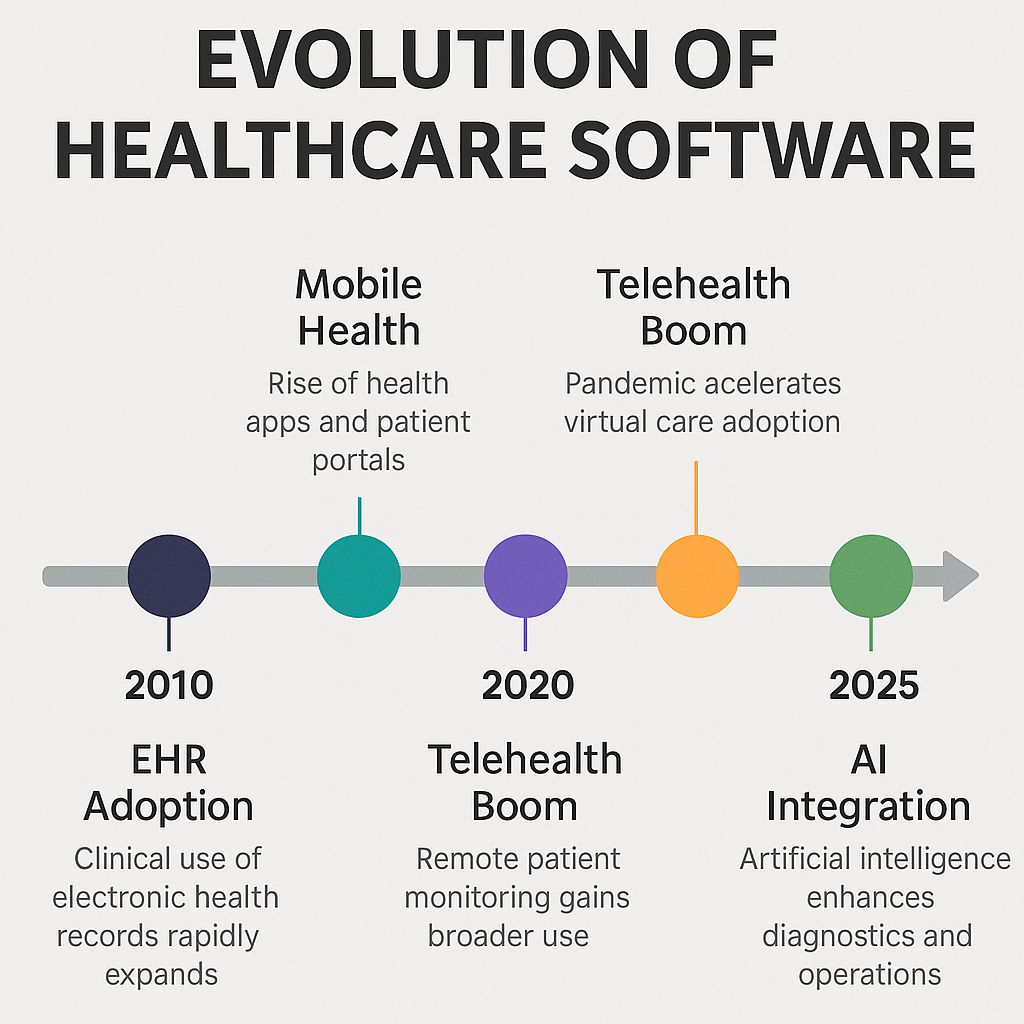
The global healthcare software market is enormous valued at over $300 billion in 2023 and projected to exceed $600 billion by 2028 – and it’s growing fast. This surge is driven by real needs: improving patient outcomes, reducing paperwork, ensuring regulatory compliance, and cutting costs.
Whether you’re a hospital administrator looking to boost efficiency, a health tech startup seeking the next innovation, or a software developer building medical applications, understanding the landscape of healthcare software is crucial.
10 Types of Healthcare Software in 2025
Now, let’s dive into the top10 types of healthcare software shaping the industry in 2025. For each, we’ll explain what it is, how it’s used, and share real-world examples and insights on making the most of it.
-
Electronic Health Records (EHR) Systems
-
Telemedicine Software
-
Remote Patient Monitoring (RPM) Software
-
Medical Diagnosis Software (AI Diagnostics)
-
Clinical Decision Support Systems (CDSS)
-
Hospital Management Systems (HMS)
-
Revenue Cycle Management (RCM) Software
-
Patient Portals and Engagement Platforms
-
Medication Management Apps
-
Mobile Health Apps (mHealth)

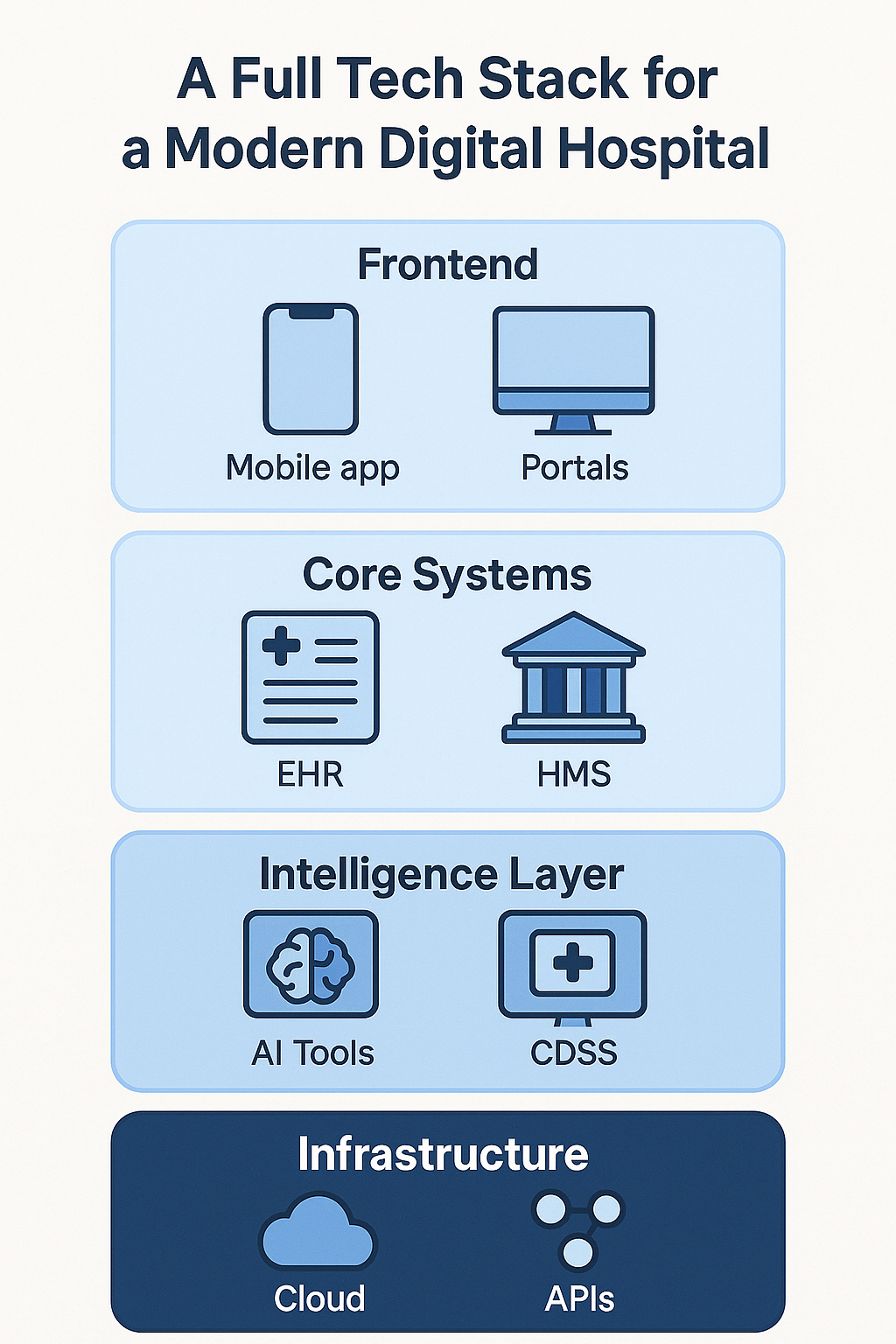
1. Electronic Health Records (EHR) Systems
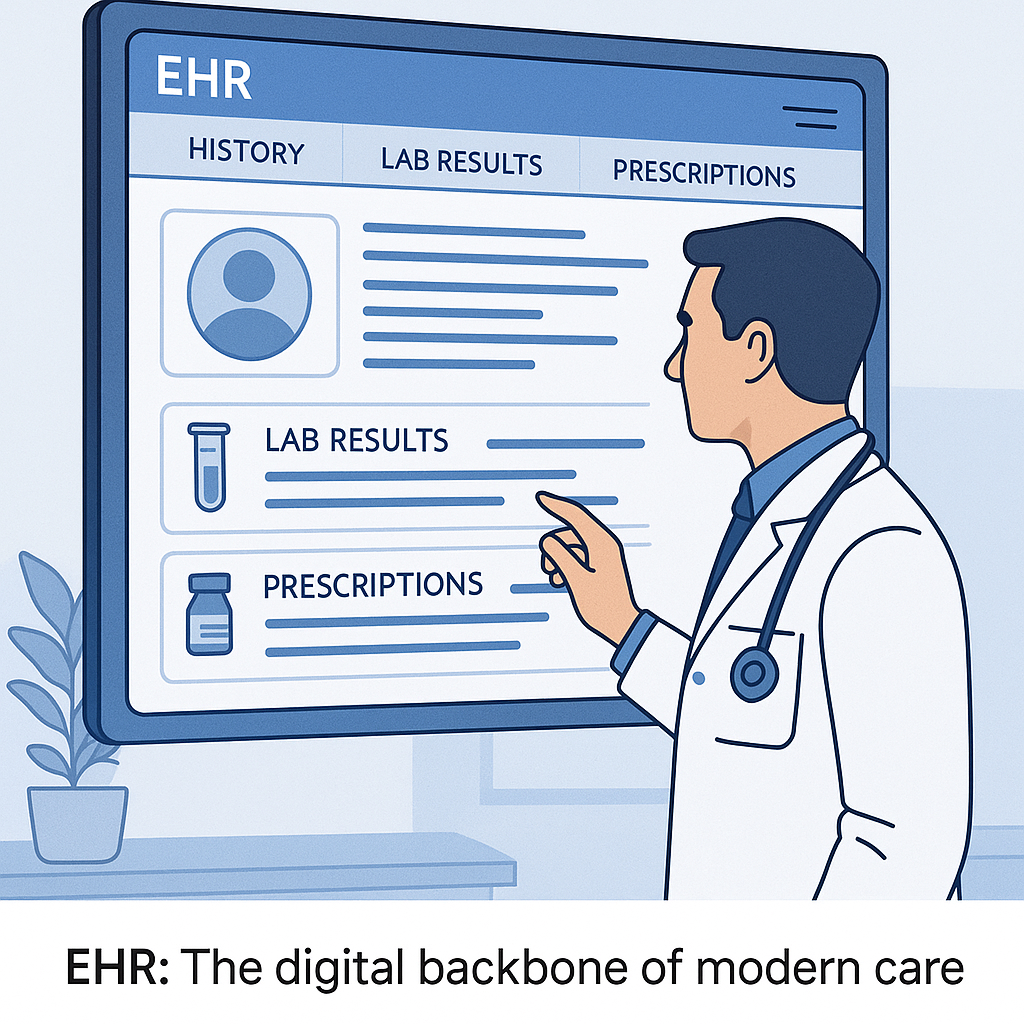
Remember the walls of paper charts in doctors’ offices? Electronic Health Record (EHR) systems have largely replaced those, becoming the central nervous system of modern clinical practice. An EHR is a digital system for maintaining patient medical histories, diagnoses, medications, treatment plans, immunization dates, allergies, radiology images, lab results essentially all the key medical information about a patient under one roof.
Unlike old paper files, EHRs are designed to be easily shared (securely) across different healthcare providers, so wherever a patient goes, their data can follow.

For example, if you visit a specialist, with a few clicks they can see the blood tests your primary doctor ordered last month, rather than ordering duplicates. This not only improves care continuity but also reduces errors (no more guesswork because someone’s handwriting was illegible!) and saves time.
According to the Office of the National Coordinator for Health IT (ONC), more than 95% of U.S. hospitals use certified EHR systems. In the EU, adoption is also high, though it varies by country (some countries have nationwide EHR systems, others more fragmented).
Two terms often heard alongside EHR are EMR (Electronic Medical Record) and EPR (Electronic Patient Record). They are related concepts: an EMR usually refers to a digital record within one provider’s office (like the digital version of a chart at a single clinic), whereas an EHR is more comprehensive and meant to travel with the patient across providers. Some hospitals use EPR to mean an internal record system, but broadly, “EHR” is the term for the integrated, longitudinal record.
 Systems.avif)
What makes EHR software so powerful is not just data storage, but decision support and workflow integration. Modern EHRs include features like: alerts for potential medication allergies or drug interactions when a doctor tries to prescribe something (this ties into the Clinical Decision Support we’ll discuss next); templates for common clinical notes to save time, built-in billing and coding assistance, and patient portal access (so patients can view parts of their record online).
A well-known example is Epic or Cerner – if you’re in the healthcare IT world, you know these giants. In fact, if you go to a large U.S. hospital, there’s a good chance your data sits in an Epic EHR. In Europe, you might encounter systems like System C in the UK or regional platforms like France’s Dossier Médical Partagé.
Why it matters
A Journal of Patient Safety study showed a 70% reduction in medication errors after EHR implementation.
However, they are not without challenges. Many clinicians initially complained about clunky interfaces and extra time spent clicking checkboxes, leading to user fatigue. The industry has responded by investing in better user experience and voice recognition (doctors can dictate notes rather than type) and by improving interoperability (making different EHR systems talk to each other seamlessly).
For Hospital Administrators
For hospital administrators, an EHR is likely the biggest IT investment and one of the most mission-critical systems. Ensuring proper training and configuring the software to match clinical workflows is crucial – a poorly implemented EHR can frustrate staff, whereas a well-tuned one can significantly boost efficiency and care quality.
Read: Custom Healthcare Software Development in South Africa
In the U.S., new regulations (like the 21st Century Cures Act) push for patients to have easy access to their records and for systems to share data via APIs. In the EU, initiatives for cross-border health data exchange are underway.
Ready to build your custom healthcare software? Contact us today
This means if you’re a software developer, skills in standards like HL7 FHIR (a modern standard for exchanging health records electronically) are highly valuable. Ultimately, the EHR is the backbone of healthcare IT – connecting to almost every other software on this list and it’s a field where experience, clinical understanding, and careful attention to privacy/security (like access controls and audit logs to prevent data breaches) are absolutely essential.
2. Telemedicine Software
Can you imagine visiting your doctor without leaving home? That’s exactly what telemedicine software makes possible. Telemedicine (or telehealth) platforms enable healthcare providers to consult with patients via secure video conferencing, voice calls, or even text/chat. In essence, it virtualizes the doctor’s visit.
By 2025, telemedicine is not just an experiment – it’s a booming industry. According to Grand View Research, the U.S. telehealth market is projected to reach approximately $64 billion by 2025, a figure boosted by the pandemic and continuing demand for convenient care.
Across Europe and other parts of the world, telemedicine has likewise become a key part of healthcare delivery, especially in regions with remote populations or where specialist access is limited.
Telemedicine software typically includes a few key features: a video call interface that is often HIPAA-compliant or meets healthcare privacy standards (so Zoom or Skype won’t cut it; instead, specialized platforms like Doxy.me, Amwell, or Teladoc are used), scheduling and waiting room management (similar to a clinic, patients might check in and wait for the doctor to join), and often some form of record sharing (e.g., the ability to display test results or images to the patient, or have them fill a questionnaire beforehand).
Many telehealth tools also integrate e-prescribing and billing, so after your virtual consultation, the doctor can send a prescription to your pharmacy and charge your insurance just as if you came in person.
The beauty of telemedicine is how it breaks down geographical barriers. A patient in a rural area can connect with a specialist in a big city without a 5-hour drive. A working parent can have a pediatrician check their child’s rash over video during a lunch break. It also proved invaluable in keeping care going during COVID-19 lockdowns.
Telemedicine isn’t suitable for every situation – you can’t set a broken bone or do a throat swab for strep via video (yet) – but it works very well for many follow-ups, minor illnesses, mental health counseling, and even physical therapy coaching sessions or post-surgery check-ins.
Healthcare provider insights
Many clinicians who were initially skeptical of “video medicine” have been pleasantly surprised by how effective it can be. A common story: a specialist had a patient travel hours for a 15-minute follow-up that could easily have been done online. Now, they conduct that follow-up via telehealth, saving the patient a trip and freeing up office resources.
Hospitals and practices are now often setting up dedicated telemedicine clinics, with some staff focusing on virtual visits. The U.S. and several European health systems have updated reimbursement policies to pay for telehealth visits more regularly, which was a big factor in adoption (pre-2020, one barrier was that a video visit might not be reimbursed like an office visit – that’s changing rapidly).
From a development standpoint, telemedicine software needs to be user-friendly (for potentially non-tech-savvy patients), reliable (glitchy video or frequent disconnects can ruin a visit), and secure (private medical info is being discussed and shown).
Features like one-click join (no complicated setup for patients), multi-party calls (for example, bring in an interpreter or a family member remotely), and integration with medical devices (like a Bluetooth stethoscope or blood pressure cuff data) are evolving.
As telemedicine becomes routine, another focus is interoperability with EHRs – doctors want the video visit documentation, plus any patient-uploaded photos or data (like a picture of a rash, or readings from a home glucometer) to flow into the main health record.
Standards like HL7 FHIR are helping with that. For healthcare organizations, choosing a telemedicine platform involves considering scale (how many concurrent visits it can handle), compliance, and ease of use.
Many EHR vendors now have built-in telehealth modules, but standalone specialized vendors can offer more features. One actionable takeaway: telemedicine is here to stay, so investing in a robust system and training your staff to use it effectively is wise.
It can improve access, keep patients engaged, and even open up new service lines (like offering tele-psychology or dietician consults that you might not have had on-site). Telemedicine software truly turns “healthcare anywhere” into a reality.
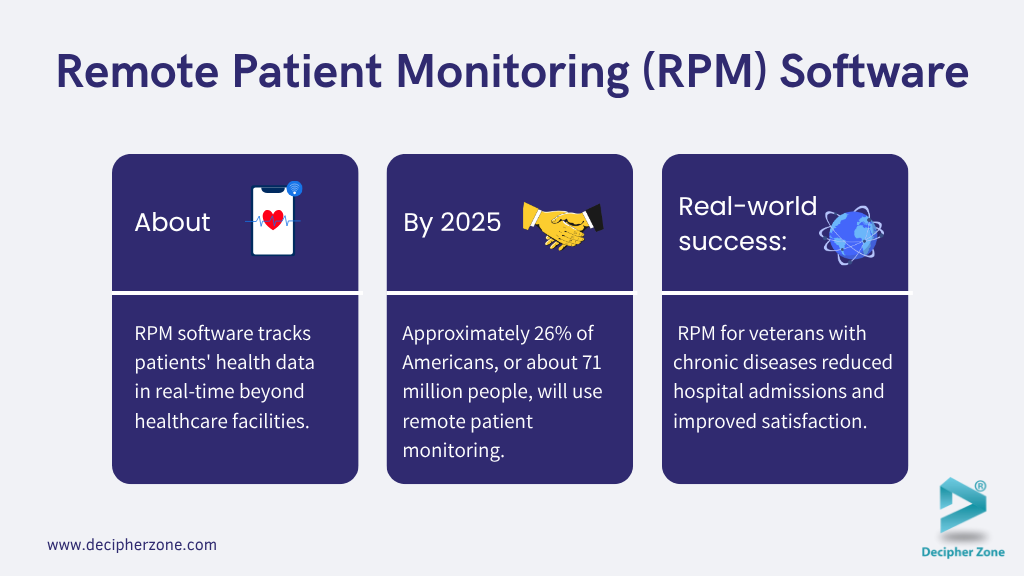
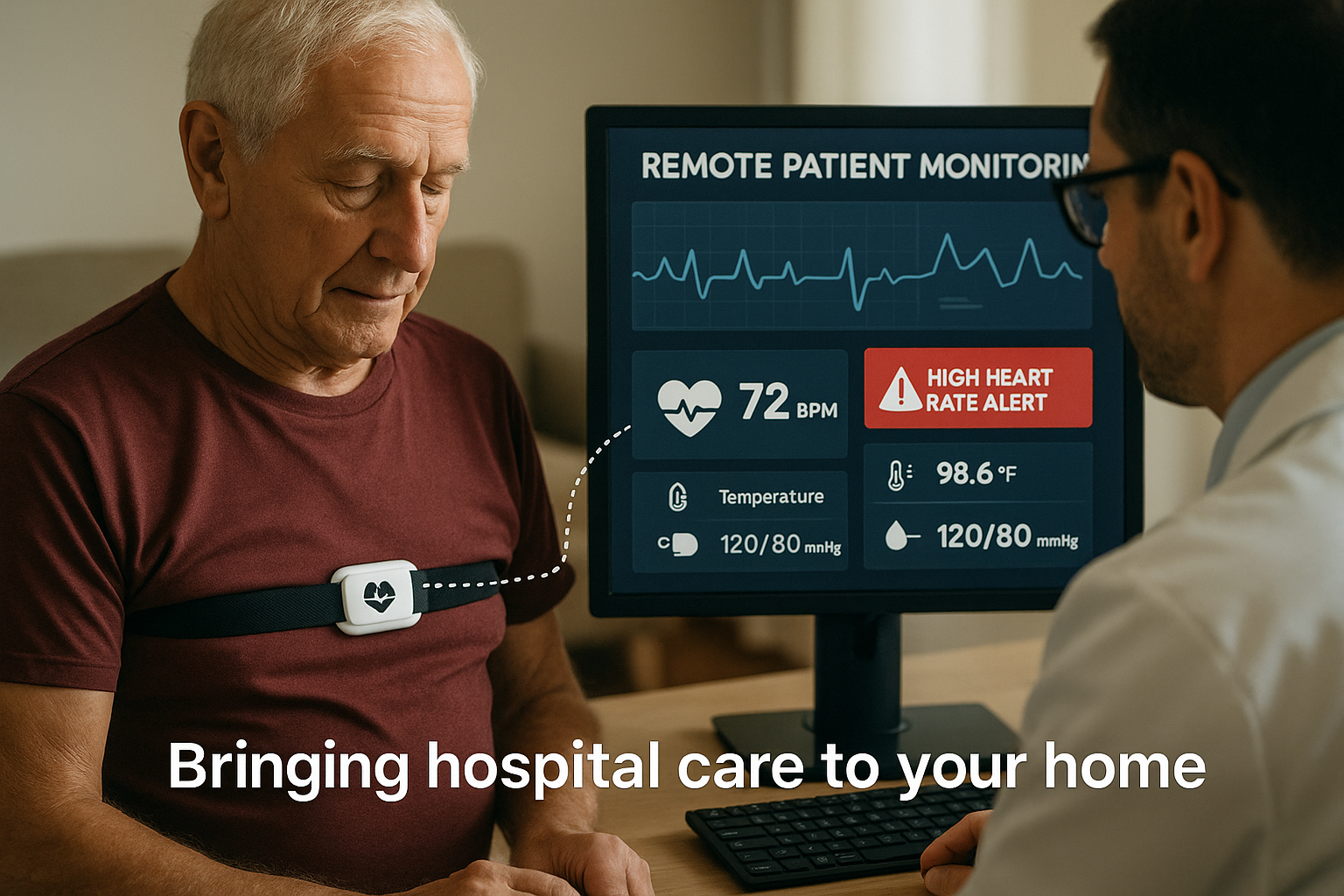
3. Remote Patient Monitoring (RPM) Software
Remote Patient Monitoring software extends the reach of healthcare beyond the clinic or hospital and into the patient’s daily life. RPM involves using connected devices and software to track patients’ health data in real-time when they’re not physically present in a healthcare facility.
This type of software gathers measurements such as blood pressure, blood glucose, heart rate, oxygen saturation, weight, or even activity levels from patients—often via wearable sensors or at-home devices and securely transmits that data to healthcare providers.
The goal is to keep a continuous or regular check on patients’ conditions and catch any warning signs early. Think of it as a virtual nurse that checks in on you and alerts your doctor if something seems off.
In practical terms, consider a patient with chronic heart failure. After a hospitalization, they’re sent home with a smart scale and a blood pressure monitor that connects to an RPM app. Each day, their weight and blood pressure readings are automatically sent to their clinic.
Sudden weight gain could signal fluid retention (a sign of heart failure worsening), and the care team would get an alert to call the patient or adjust medications before it escalates to an ER visit.
Another example: a diabetic patient uses a continuous glucose monitor (CGM) patch on their arm, which sends glucose readings to an app viewed by their endocrinologist. If their sugars go dangerously high or low, the system flags it. In maternity care, some programs send expectant mothers home with blood pressure cuffs to catch early signs of preeclampsia. The applications are vast.
By 2025, RPM has become a huge trend – partly spurred by COVID-19 forcing remote care, and partly by advancing tech. A study by Insider Intelligence projects that approximately 26% of Americans, or roughly 71 million people, will use remote patient monitoring by 2025.
Globally, hundreds of millions of data points are being collected via these programs. Not only does RPM improve individual patient care, but it’s also a way to manage population health.
For example, a health system can enroll thousands of hypertension patients in a monitoring program to help keep their blood pressure in check, reducing strokes and heart attacks in the long run.
For Hospital Administrators
For hospital administrators, adopting RPM can reduce readmissions and free up beds. Patients who might have been kept longer for observation can potentially go home sooner if they’re monitored remotely.
It also enhances patient satisfaction because people generally prefer to recover at home rather than staying in a hospital. Importantly, reimbursement has been catching up: in the U.S., Medicare and many private insurers now reimburse for certain RPM services, acknowledging their value.
For Developers
From a tech perspective, RPM software needs to handle device integration (working with various health IoT devices from blood pressure cuffs to pulse oximeters), data streaming and storage (often large volumes of time-series data), and analytics/alerting.
Many systems include a clinician dashboard where nurses or doctors can see trending charts and receive alerts when readings fall outside preset parameters.
Some incorporate patient self-management tools too—like medication reminders or educational content triggered by the readings (e.g., if your blood sugar is high, the app might nudge you to check your diet or medication).
Read: Industries Benefiting from Custom Software Development
Real-world success
A large Veterans Affairs (VA) study in the U.S. found that RPM for veterans with chronic diseases significantly reduced hospital admissions and improved satisfaction.
Another example, UPMC (University of Pittsburgh Medical Center) reported that their remote monitoring program cut hospital readmissions by 76% for heart failure patients and achieved patient satisfaction over 90%. These are huge improvements, demonstrating that when done right, RPM can lead to better outcomes and happier patients.
For Developers and Startups
For developers and startups, RPM is a fertile ground but requires deep understanding of both technology and clinical workflows. Ensuring data accuracy and reliability is paramount devices need to be vetted (FDA approved if in U.S.), and connectivity must be robust (what if an elderly patient’s internet drops? The system should handle gaps gracefully).
User experience is also key: devices have to be easy to use for patients of all backgrounds, and the software interface for clinicians should help them prioritize attention (perhaps via AI that filters signal from noise, so clinicians aren’t overwhelmed by data).
Privacy is another concern: constant data flow means ensuring that data is encrypted and only accessible by authorized folks, aligning with GDPR, HIPAA, etc.
Need top developers for your next health tech project? Let’s partner for success in digital health
Overall, RPM software embodies the proactive, preventative approach modern healthcare is striving for catching small issues before they become big problems by keeping a digital finger on the patient’s pulse, literally and figuratively.
4. Medical Diagnosis Software (AI Diagnostics)
Diagnosing an illness is sometimes like solving a puzzle: the pieces are symptoms, history, exams, and tests, and the doctor’s job is to put them together correctly.
Medical diagnosis software aims to assist in this process, often using advanced AI algorithms. These tools can comb through vast amounts of data – from medical literature, databases of case histories, and even real-time patient data to suggest possible diagnoses that a clinician might consider.
One way to think of it: it’s like having a well-read assistant whispering in your ear, “Have you considered this rare condition? In cases similar to this, it turned out to be X.”
"Dr. John Smith, Chief Medical Officer at HealthAI, highlights, 'AI-based diagnostic tools are essential companions for clinicians, significantly reducing misdiagnosis rates, especially in complex cases."
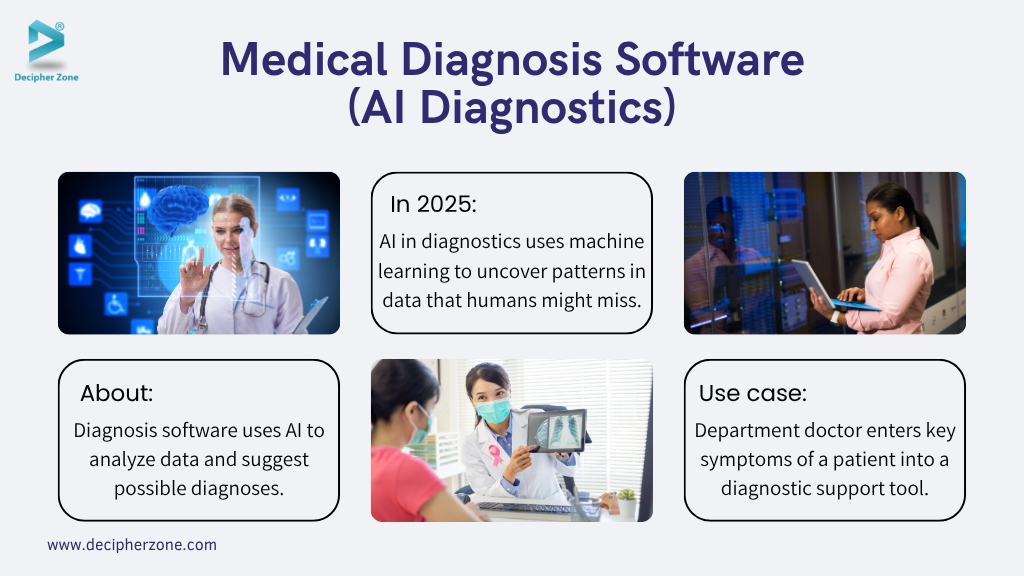
There are a couple of flavors of diagnostic software. For healthcare professionals, some platforms allow doctors to input patient information (symptoms, lab results, demographic details) and then generate a list of potential diagnoses ranked by likelihood.
This is particularly useful for complex cases or rare diseases that a doctor might not encounter often. It doesn’t give a definitive answer, but it can broaden the differential diagnosis.
For example, a physician in a remote area could use such software to get input on an unusual combination of symptoms, ensuring they don’t miss an uncommon disease. Some well-known systems over the years include Isabel and DXplain, and more recently various AI-driven apps.
There are also consumer-facing diagnostic apps, essentially symptom checker apps for individuals. You’ve probably seen or used one: you answer a questionnaire about what you’re feeling, and the app uses a database (and sometimes AI) to tell you possible causes or whether you should see a doctor.
During the pandemic, these became popular to distinguish COVID-19 from cold or flu symptoms. Apps like Ada, Babylon Health, or WebMD’s symptom checker are examples.
They ask things like “Do you have a fever? Difficulty breathing?” and then give guidance (“It could be XYZ, consider getting a COVID test or seeing a provider”). These aren’t meant to be final diagnoses, but they can help guide people on next steps.
In 2025, AI in diagnostics is a hot area. Machine learning models can find patterns in data that humans might miss.
Real Use Cases
A busy emergency department doctor has a patient with a confusing set of symptoms. They quickly input the key info into a diagnostic support tool. The software suggests considering a rare metabolic disorder that the doctor hadn’t initially thought of, given some abnormal lab values.
The doctor orders a specific test for that disorder and it comes back positive, enabling a correct diagnosis and treatment that might have otherwise been delayed. This kind of assistive tech can be literally life-saving in such scenarios.
For Healthcare Leaders, Startups and Developers
For healthcare leaders, adopting diagnostic software can mean better outcomes and fewer missed diagnoses, but it must be done carefully. Clinicians need training to use these tools effectively and to understand their limitations (AI can have biases or make odd errors).
For startups/developers in this space: it’s crucial to validate your algorithms with solid clinical evidence and to collaborate with medical experts. Acceptance in the medical community will depend on showing that your tool actually improves diagnostic hit rates or efficiency. Also, be mindful of regulatory oversight an app that effectively diagnoses conditions likely falls under medical device regulations.
But it’s a field with immense promise. As the saying goes, “Two heads are better than one,” and diagnosis software is like adding a super-computerized second head to the diagnostic process. Used wisely, it can increase confidence and thoroughness in figuring out what’s ailing a patient.
5. Clinical Decision Support Systems (CDSS)
Healthcare is complex, and even the best clinicians appreciate some backup. Clinical Decision Support Systems (CDSS) are software tools that provide intelligent assistance to doctors, nurses, and other healthcare professionals in making clinical decisions.
Research published in the BMJ Quality & Safety Journal found that CDSS significantly improves clinical outcomes by reducing adverse drug events.
They essentially analyze patient data and medical knowledge bases to offer alerts, reminders, or recommendations at the right time. A simple example: when a doctor prescribes a new medication, a CDSS module in the EHR might pop up an alert if the patient’s record shows an allergy to that drug, or if it may negatively interact with another medication the patient is taking.

Another example: a primary care doctor enters a patient’s symptoms and lab results, and the system suggests considering a particular diagnosis or ordering a certain test that might be relevant. These suggestions are typically based on clinical guidelines, research, or patterns learned from large datasets.
The goal of CDSS is not to replace the provider’s judgment, but to augment it with data-driven insights. Clinicians deal with an immense amount of information and ever-updating medical research. CDSS tools can help by flagging important nuances that a human might overlook especially in fast-paced environments.
Modern decision support often involves AI and machine learning. Some systems can learn from historical patient outcomes to predict what treatments might work best for a current patient.
For example, an oncology CDSS might compare a cancer patient’s genetic profile and tumor characteristics with thousands of past cases to suggest which chemotherapy regimen has the best success probability.
Another domain is imaging: AI-based CDSS can analyze radiology images (like x-rays or CT scans) and highlight suspicious areas for the radiologist to review, acting as a second set of eyes.
Real-world impact
A well-known CDSS example is the drug interaction checker integrated in most EHRs – it has undoubtedly prevented countless adverse drug events by catching conflicts. Another is IBM’s Watson for Oncology (a famous AI that digested medical literature to suggest cancer treatments, though its real-world performance had mixed reviews).
Even simpler, many clinics have built-in decision rules, like “if a patient has diabetes and hasn’t had an eye exam in a year, remind the doctor to refer them to an ophthalmologist.” These little reminders ensure preventive care steps aren’t missed.
Studies have shown CDSS can improve adherence to guidelines and reduce errors, but they must be carefully managed too many alerts can lead to “alert fatigue” where providers start ignoring them. So, implementers need to fine-tune what triggers an alert, making sure each interruption is truly valuable.
For Developers and Startups
The CDSS space is exciting and challenging. It sits at the intersection of medicine, data science, and human factors design. You not only need good algorithms, but you also must integrate into clinical workflows seamlessly. No doctor wants a clunky pop-up in the middle of writing a note that doesn’t clearly help.
Successful CDSS solutions often involve close collaboration with clinicians to ensure the support is relevant and presented at the right time. Also, any CDSS that provides treatment recommendations might be considered a medical device by regulators (like the FDA or EU’s CE marking), which means rigorous validation is required.
Have questions? Chat with us on WhatsApp
But when done right, clinical decision support systems are like a safety net and an expert consultant rolled into one – helping ensure that every patient gets care that’s informed by the latest knowledge and tailored to their personal data.
6. Hospital Management Systems (HMS)
Running a hospital is incredibly complex – it’s like running a small city that operates 24/7, with lives on the line. Hospital Management Systems (HMS), also known as Hospital Information Systems (HIS), are comprehensive software suites designed to handle the administrative, financial, and operational needs of a hospital.
According to a Healthcare Information and Management Systems Society (HIMSS) report, integrated HMS systems have streamlined hospital operations, improving efficiency by up to 40%.
If an EHR focuses on patient clinical information, and HMS zooms out to manage the hospital’s logistics and workflows at large. These systems often include modules for patient registration, admission & discharge, bed management, staff scheduling, billing, inventory (for medications and supplies), and reporting. Essentially, HMS is the backbone that keeps the hospital running smoothly behind the scenes.
Consider what happens when a patient comes to an Emergency Department: the HMS registers them, assigns a medical record number, maybe even an initial triage category. If admitted, the system assigns a bed and notifies the ward staff. It tracks that patient’s journey any tests ordered, their movement from ER to ICU to a regular ward, and eventually discharge.
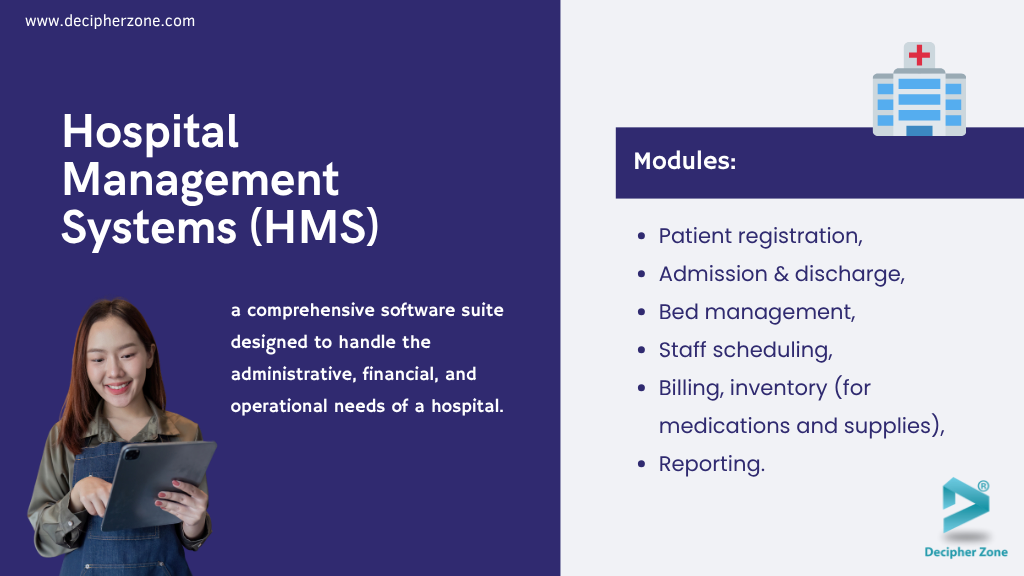
Simultaneously, the billing module is tallying charges (room fees, medications used, procedures done) and generating claims for insurance. In parallel, the inventory module might flag that the ICU is down to the last two units of a certain medication after this patient’s use, prompting the pharmacy to restock. All this is coordinated via a central system.
Read: Digital Transformation in the Healthcare Industry
One of the huge advantages of a good HMS is efficiency and error reduction. For example, a quality HMS will ensure that when a doctor orders a lab test in the EHR, it’s linked to the billing and inventory – so the lab knows it’s authorized, the cost is captured, and if it’s a rare test, the system knows to stock up the necessary kit.
Bed management is another critical aspect: knowing in real-time which beds are occupied, which are being cleaned, and where new patients can be placed. This was vital during COVID surges – hospitals had to have a tight grip on bed availability and oxygen supply, etc., which many HMS have dashboards for.
HMS often integrate or interface with other software: EHRs, radiology systems, lab systems, pharmacy systems. In some cases, the HMS and EHR are part of one giant platform (many big vendors offer an all-in-one). In other cases, a hospital might piece together the best of each and ensure they talk to each other via interfaces.
For example, when a lab result is ready in the lab system, it flows into the HMS/EHR so that clinicians see it, and at discharge, the HMS might compile a summary for the patient. The billing and claims part of HMS is particularly complex in places like the U.S. due to insurance – these systems help coders assign proper ICD codes, apply insurance rules, and send electronic claims.
In Europe, with more centralized or public healthcare, billing might be simpler, but they still track costs and resource usage for internal budgeting and national health service reporting.

Use Case Example
A hospital using an HMS can implement automatic alerts like: if a patient has been admitted for 30 days (a long stay), trigger a case manager review; or if an operating room is running past schedule, notify the next surgery team of the delay via the system.
Another scenario: a patient is ready to be discharged but their take-home medications need to be prepared – an HMS could integrate with the pharmacy system to ensure those meds are delivered to the ward on time, and notify housekeeping to clean the bed for the next patient as soon as discharge orders are in.
For Hospital Administrators
An HMS provides a bird’s-eye view through dashboards: current patient count, occupancy rate, staff on duty, revenues, etc., and can generate regulatory reports. It’s indispensable for compliance as well (like keeping logs for accreditation or government audits).
One actionable insight is that implementing an HMS is not just an IT project, but a change management one it touches every department, so training and gradual adaptation are key.
Also, customization is often needed: each hospital might have slightly different workflows (a teaching hospital might need to track which cases go to which teaching units, etc.).
From a technology standpoint, many modern HMS are moving to cloud-based or hybrid models. Security is paramount, as these systems hold not just patient health info but also financial data and personal identifiers. In the EU, data residency and GDPR compliance might influence whether a cloud HMS is allowed or if it stays on-premise.
For Developers and Vendors
For developers and vendors, staying compliant with standards (like HL7, ICD-10 coding, etc.) and being able to integrate with a myriad of devices (even IoT, like connecting to smart infusion pumps or patient wristband trackers) can set your system apart.
Bring your healthcare vision to life — Explore our web app development services
Ultimately, a robust Hospital Management System ensures that clinicians can focus on patient care while the system quietly handles the orchestrations of hospital operations, reducing administrative burdens and minimizing mistakes in the hustle and bustle of healthcare delivery.
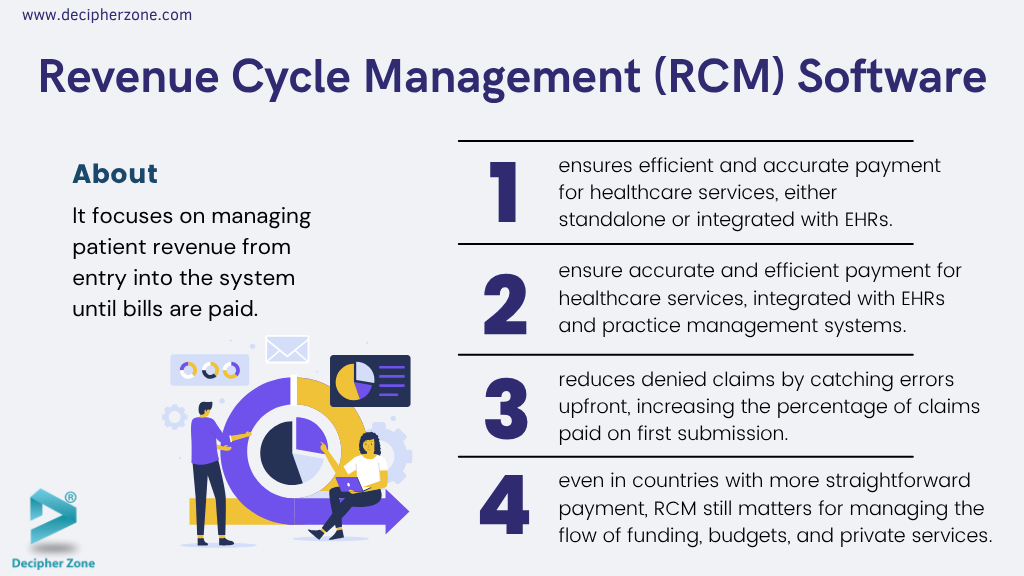
7. Revenue Cycle Management (RCM) Software
Healthcare is about healing and helping, but it’s also a business – and a complex one at that. Revenue Cycle Management (RCM) software focuses on the financial side of healthcare, specifically the process of tracking and managing the revenue from patients from the moment they enter the system until their bills are paid.
As stated by the Medical Group Management Association (MGMA), effective RCM software can improve first-pass claim acceptance rates by as much as 90%.
The “revenue cycle” covers everything from appointment scheduling and insurance verification, to coding of services, to billing, and finally collections. RCM software either stands alone or is integrated with systems like EHRs and practice management systems to make sure healthcare providers get paid for the services they deliver, and that it’s done efficiently and accurately.
Imagine a patient’s journey: they schedule an appointment RCM starts right there by checking their insurance eligibility (is their policy active? what’s covered? what co-pay might apply?).
When they receive care, every service, procedure, test, medication may translate to billing codes (like CPT, ICD-10, etc.). Proper documentation in the EHR is coded and fed to the RCM system.
The RCM software then creates a claim to send to the patient’s insurer, following all the rules and formats required. It might also cross-check that the codes used match the diagnosis (insurance won’t pay for a test that doesn’t have an appropriate diagnosis code justifying it, for instance). If something’s off, good RCM software will flag it before submission, avoiding a denial.
Once the claim goes out, the software tracks it. If the insurer responds, maybe they pay some and deny some – the RCM system logs that, and possibly triggers actions like “need to appeal denial” or “bill patient for co-insurance”.
If insurers don’t respond in a timely way, it reminds billing staff to follow up. For patient-billed balances, it can issue invoices, process payments, set up payment plans, and even manage collections for overdue accounts.
Why is this such a big deal? Well, in the U.S. especially, the process of getting paid is notoriously complicated. Administrative costs are a significant part of healthcare expenditures. A strong RCM system can reduce the number of denied claims by catching errors upfront (missing info, wrong code, etc.), thus increasing the percentage of claims that get paid on first submission.
It can also speed up payments – if you verify insurance and know the patient’s share at the visit, you can collect co-pays immediately, and send clean claims out the next day rather than dealing with them weeks later. Over the entire cycle, this means better cash flow for a clinic or hospital.
Even in countries with more straightforward payment (like single-payer systems), RCM still matters for managing the flow of funding, budgets, and any private services.
In many EU countries, for example, public hospitals might still bill various entities or handle cross-border billing through EU health insurance cards, etc. And private clinics definitely use RCM to manage private insurance and patient payments.
RCM software often provides analytics: dashboards that show, for example, the total accounts receivable, average days in A/R (how long it takes to get paid), denial rates, etc.
A hospital CFO might look at these daily. If an RCM report shows a spike in denials due to some code, they can investigate – maybe a new medical coder needs training, or a rule changed in insurance and now a different code is needed.
Read: Dental Software Development Cost
Use case insight
Let’s say a clinic implements a new RCM system. They discover through its tools that many claims were being denied because referrals or pre-authorizations were missing.
The RCM now integrates a step where, at scheduling, it prompts staff: “Does this appointment need a referral or pre-auth? If yes, ensure it’s obtained.” In a few months, their denial rate drops, and revenue improves because fewer services go uncompensated.
RCM software might also incorporate patient price transparency tools, generating estimates so patients know what they might owe ahead of time. This is increasingly important as regulations push providers to be upfront about costs.
Some advanced RCM platforms even integrate a bit of patient CRM (Customer Relationship Management), sending reminders about balances or offering online payment portals for convenience.
 Software.avif)
For Developers and Startups
For tech folks and startups, RCM can sound a bit dry, but it’s ripe for innovation. The use of AI to predict which claims might get denied or to automate posting of payments (reading remittance advice documents from insurers) can save human hours.
Robotic Process Automation (RPA) is used in some revenue cycle departments to do repetitive tasks like checking claim status on payer websites. Security and compliance (like HIPAA) are obviously crucial since financial records tie to patient info.
And any solution must adapt to constantly changing insurance rules and codes. Interoperability (with EHRs, clearinghouses, national health systems) is key too.
8. Patient Portals and Engagement Platforms
In the past, patients were often passive recipients of care, but today they’re increasingly taking an active role in managing their health. Patient portals are a key tool enabling this shift.
A patient portal is a secure online platform (usually a website or mobile app) where patients can access their personal health information and interact with healthcare services. Typically connected to an EHR or hospital system, portals let patients do things like view their test results, schedule appointments, request prescription refills, send messages to their doctors, and sometimes even have e-visits.

Imagine you had blood tests done instead of waiting days for a call, you get a notification and can see the results on your phone along with an explanation of what’s normal or not. You notice your cholesterol is a bit high through the portal, you send a message to your doctor asking if you should be concerned.
The doctor replies the next day with some advice all without playing phone tag. That’s a common portal interaction. Portals often also hold documents like visit summaries, vaccine records, and discharge instructions, so you have your health info at your fingertips.
For appointment management, portals are super handy: a lot of clinics enable online booking or at least requesting appointments through the portal. You can also fill out intake forms or update your medications list from home, which saves time during the visit. Billing is another feature – many portals show your statements and let you pay bills online securely.
The value of portals in 2025 is widely recognized. In the U.S., a huge push came from federal “Meaningful Use” incentives that required offering portals to patients; now almost all major health systems have them.
In the EU and UK, patient access to records is a core part of digital health strategies (like NHS’s online services or Estonia’s nationwide e-health portal). By 2022, around 60% of U.S. adults had been offered a portal and about half actually used it.
Usage is climbing, especially as younger, tech-savvy generations expect digital convenience. However, challenges remain (some people find sign-up cumbersome, or worry about privacy, or just prefer phone).
A portal is more than a static repository – the newer ones are becoming interactive health management tools. For example, a portal might show personalized health reminders: “You’re due for a mammogram” or “Time to schedule your annual diabetes check-up.” Some integrate educational content linked to your conditions – e.g., you have asthma, so the portal suggests an article or a short video on inhaler techniques.
It’s about keeping patients engaged in their care, which studies have shown can lead to better outcomes (patients who read their visit notes and understand their plan are more likely to follow through).
Want a tailor-made mobile solution? Check out our mobile app development
Use Case Example
An example scenario of impact: A patient with hypertension logs daily blood pressure readings into their portal (some portals allow manual entry or even device syncing). The clinic’s nurse monitors a list of portal inputs and sees this patient’s readings are high this week. They send a portal message advising an adjustment in diet and schedule a follow-up call.
The patient, meanwhile, might use the portal’s chatbot (some advanced ones have symptom checkers or bots) to ask about a side effect of their medication, getting instant info at midnight. These interactions demonstrate a level of continuous care that wasn’t possible before.
From a tech perspective, portals must be user-friendly and secure. They are patient-facing, so design and simplicity are huge – if it’s confusing, patients won’t use it. Mobile-friendliness is non-negotiable now.
Multi-factor authentication is common to protect access (sensitive info is inside!). And portals have to respect privacy preferences; for example, some adolescents have parts of their record that parents shouldn’t see (like sexual health info by law), so portals implement nuanced access control.
Read: software development
For Developers
Integration is also key: the portal needs to pull data from the EHR in real-time or near real-time. Standards like FHIR have made it easier for third-party apps to serve as patient portals, but many healthcare systems use the portal offered by their EHR vendor (like Epic’s MyChart, which is very widespread, or Cerner’s HealtheLife). T
here’s also a trend of personal health record apps (PHRs) that let patients aggregate data from multiple providers – some patients have several portals (one for each specialist or hospital) which is a pain new solutions like Apple Health Records on the iPhone use FHIR to pull from multiple sources into one place for the patient. This isn’t exactly a portal itself, but it’s patient-controlled access to data.
Challenges like digital literacy and trust need addressing: some people are uneasy with online records. Clear communication about security and benefits helps.
Also, as found in surveys, a chunk of patients just prefer human interaction or worry about misunderstanding results if doctors aren’t there to explain. That’s why many portals release results either with a short delay to let doctor review or with accompanying explanations.
For Healthcare Providers
For healthcare providers, the portal can reduce clerical burdens (less calls for results or scheduling) and improve patient satisfaction. But it also introduces tasks like answering patient messages timely. Many clinics set up protocols: e.g., nurses handle routine questions, doctors see others. Some even bill for certain e-visits through portal messaging if it substitutes a visit.
9. Medication Management Apps
Taking medications correctly is a cornerstone of effective healthcare – yet it’s surprisingly hard for many patients. Medication management apps are designed to tackle this very problem.
They help patients organize, remember, and understand their medications. A classic function is the pill reminder: the app sends you a notification when it’s time to take your next dose, ensuring you don’t forget or double-dose. But the best medication management apps go further.
They allow users to input all their prescriptions (and over-the-counter drugs or supplements), track doses taken, and even log how they’re feeling on a medication. Some apps can alert users about potential drug interactions or provide information on side effects and proper usage.
Consider an elderly patient on multiple medications (a common scenario): Keeping track of 5, 10, or 15 pills a day is daunting. A medication app becomes essentially a personal pharmacist in your pocket. It can have each medicine’s name, an image of the pill, dosing instructions, and refill dates.
When the patient visits their doctor, they can show the app’s list to quickly review everything they take – avoiding the “shoebox full of pill bottles” confusion. Many apps also allow caregivers or family members to be connected. For example, an adult child could get an alert if their aging parent misses a dose, enabling them to follow up.
For Healthcare Providers
From the healthcare provider perspective, medication adherence (i.e., patients taking meds as prescribed) is a huge deal. Non-adherence is linked to poorer outcomes and higher hospitalizations.
By improving adherence rates, these apps can literally save lives and reduce healthcare costs. In one success story, a clinic implementing a medication reminder app for cardiac patients saw significantly fewer readmissions for heart failure, as patients were taking their meds more reliably.
For startups, this field has some established players (like Medisafe, a popular medication reminder app), but there’s room for innovation especially in integrating with pharmacies and EHRs.
Imagine an app that not only reminds you to take your pill but also notifies you when you’re running low and lets you reorder a refill with one click. In fact, many pharmacies in the U.S. and Europe now offer apps that combine medication management with direct refill requests.
Read: On-demand Medicine Delivery App
For Hospital Administrators
If you’re a hospital administrator, consider recommending a trusted medication management app to patients with complex regimens (some hospitals even develop their own branded apps for this). Ensure the app meets privacy standards and has a user-friendly interface. Also, consider the education aspect these apps can educate patients on why they need to take their meds regularly, not just remind them.
A little contextual info (“this blood thinner prevents strokes don’t skip it!”) can motivate adherence. All in all, medication management software exemplifies how thoughtful tech can address one of healthcare’s age-old challenges: helping patients follow through with the treatment plan long after they leave the doctor’s office.
10. Mobile Health Apps (mHealth)
Mobile health apps (often called mHealth apps) put healthcare in your pocket. These are smartphone applications that let patients manage aspects of their health or access healthcare services anytime, anywhere.
Think of a hospital’s patient portal, but optimized for your phone – or a digital clinic at your fingertips. With a few taps, patients can schedule doctor appointments, pay medical bills, chat with nurses or doctors, and receive lab results securely.

For example, many hospital systems in the U.S. offer mobile apps that allow patients to check their test results and message their provider directly, saving countless phone calls. In the EU, national health services have also rolled out apps for booking COVID vaccinations and storing digital health insurance cards. These convenient tools empower patients to take charge of appointments and information without needing to navigate paperwork or waiting lines.
Modern mHealth apps often integrate with core clinical systems. During a virtual consultation, a doctor can pull up your latest Electronic Health Record right within the app (with your permission) to review your history. This seamless flow of information means better continuity of care no more repeating your medical history multiple times.

Real-world Example
The MyChart app (by Epic Systems) is widely used in U.S. hospitals. Patients use it to see their test results, request prescription refills, and even do e-check-in before a visit.
Meanwhile, in the EU, France’s “Doctolib” app not only schedules appointments with doctors but also facilitated millions of teleconsultations during the pandemic. The success of these apps shows how mHealth is redefining patient engagement, making healthcare more accessible and user-friendly.
For Hospital Administrators
For hospital administrators, investing in a robust mobile app can significantly improve patient satisfaction scores. For startups and developers, the mHealth space presents opportunities – from creating niche wellness apps to improving interoperability with EHR systems – but also requires keen attention to privacy and security. A helpful tip is to ensure any mobile app handling patient data complies with HIPAA (in the U.S.) or GDPR (in Europe) standards for data protection from day one.
Let’s partner for success in digital health — Become a partner
A Quick Comparison Table of All the Healthcare Software
| Software Type | Main Function | Who Uses It | 2025 Trend |
|---|---|---|---|
| EHR Systems | Store & share medical records | Hospitals, clinics | Focus on interoperability |
| Telemedicine | Virtual doctor visits | All providers | Standard part of care |
| RPM Software | Monitor patients remotely | Chronic care, hospitals | Big growth with IoT |
| AI Diagnostics | Assist diagnosis | Doctors, clinics | Rising AI adoption |
| CDSS | Decision support | Doctors, nurses | AI-enhanced guidance |
| HMS | Manage hospital operations | Hospital admins | Cloud adoption rising |
| RCM Software | Manage billing & revenue | Admin, finance | AI for claim accuracy |
| Patient Portals | Engage patients | All providers | Value-based care driver |
| Medication Apps | Track meds & reminders | Patients, caregivers | Aging population focus |
| mHealth Apps | Wellness & health tasks | Patients | Integration with wearables |
How to Choose the Right Healthcare Software for Your Hospital in 2025
Selecting the right healthcare software can feel overwhelming, but breaking it down into clear steps makes it manageable. Here’s a simple guide to help hospitals, clinics, and startups make an informed choice:
1. Define your organization’s goals and challenges
Start by identifying your top priorities — is it improving patient care, streamlining operations, boosting financial performance, or all of these? Understand where your current systems fall short.
2. Set a realistic budget
Consider not just the licensing cost, but also implementation, integration, training, and ongoing support. Look at both upfront and long-term costs to avoid surprises.
3. Evaluate vendor reputation and reliability
Research vendors carefully. Look for client testimonials, case studies, certifications, and third-party reviews. A good vendor should also offer responsive support and regular updates.
4. Check for interoperability and scalability
Make sure the software can integrate with your existing systems (e.g., EHR, lab, pharmacy) and is flexible enough to grow with your organization’s future needs.
5. Plan for user adoption and training
Even the best software fails if staff can’t or won’t use it. Choose intuitive solutions and ensure comprehensive training is part of your rollout plan.
Conclusion
In 2025, healthcare software is no longer optional—it's fundamental. Hospital administrators, healthcare tech startups, and software developers must actively engage with this evolving landscape to ensure superior patient care and organizational efficiency.

Ready to transform your healthcare operations? Explore cutting-edge healthcare software solutions today and stay ahead in 2025.
FAQ
What are Electronic Health Records (EHR) Systems and why do hospitals use them in 2025?
Electronic Health Records (EHR) systems store, manage, and securely share patient medical data across providers. In 2025, hospitals use EHRs to enhance patient safety, improve care coordination, and ensure compliance with healthcare regulations.
How does telemedicine software work and what are its benefits in 2025?
Telemedicine software enables virtual consultations through secure video, voice, or chat platforms. In 2025, it offers patients easier access to care, minimizes travel needs, and helps providers maintain continuity of care.
What is Remote Patient Monitoring (RPM) software? Benefits & real use cases?
RPM software collects health data from devices used at home, like blood pressure monitors or glucose meters, and shares it with healthcare providers. Benefits include early detection of health problems, fewer hospital readmissions, and better chronic disease management.
How is AI medical diagnosis software transforming healthcare in 2025?
AI-powered medical diagnosis software analyzes patient data, symptoms, and test results to assist doctors in identifying conditions. In 2025, it supports faster, more accurate diagnoses, including rare diseases that might otherwise be missed.
What are Clinical Decision Support Systems (CDSS) and how do they help doctors?
CDSS tools provide real-time alerts, reminders, and recommendations based on patient data and medical guidelines. They help doctors reduce errors, follow best practices, and make smarter clinical decisions.
What is a Hospital Management System (HMS) and how does it improve operations?
A Hospital Management System (HMS) integrates and automates hospital operations, including patient admissions, bed management, billing, inventory, and reporting. It ensures smooth workflows and better resource use.
How does Revenue Cycle Management (RCM) software streamline healthcare billing?
RCM software handles billing, insurance claims, and collections from appointment scheduling through final payment. It helps reduce claim denials, accelerate payments, and improve hospital cash flow.
What are patient portals and how do they improve patient engagement?
Patient portals empower users by providing secure online access to records, test results, appointments, and provider communication, enhancing patient engagement.
How do medication management apps help patients stick to treatment plans?
Medication management apps provide reminders, track doses, and offer drug information. They help patients follow prescriptions correctly, reducing missed doses and improving treatment success.
What are mobile health (mHealth) apps and how do they support patient care in 2025?
mHealth apps give patients mobile access to appointments, records, test results, and communication with providers. They make healthcare more accessible, convenient, and user-friendly.
Author Profile: Mahipal Nehra is the Digital Marketing Manager at Decipher Zone Technologies, specializing in SEO, content strategy, and tech-driven marketing for software development and digital transformation.
Follow us on LinkedIn or explore more insights at Decipher Zone.

